7 Signs You’re Dealing with More Than Just Stress: Dysthymia and Anxiety Symptoms
Feeling down and worried most days isn’t just stress—it might be persistent depressive disorder and anxiety working together. These two mental health conditions often occur side by side, and recognizing their symptoms is the first step toward feeling better.
Persistent depressive disorder (also called dysthymia) is a form of chronic depression that lasts for years, while anxiety disorders like generalized anxiety disorder create ongoing worry and fear. When both affect you simultaneously, everyday life can feel especially overwhelming.
What Makes Dysthymia and Anxiety Different from Regular Stress?
Everyone experiences stress, but persistent depressive disorder and anxiety disorders follow different patterns. Stress comes and goes based on life events. Dysthymia creates lasting low mood that sticks around most days for at least two years, becoming a baseline of sadness that feels like part of who you are.
Anxiety disorders go beyond normal nervousness. Generalized anxiety disorder involves excessive worry about multiple life areas—work, health, relationships, money—that’s hard to control and happens more days than not.
Many people with dysthymia also have comorbid anxiety disorders. When these mental health conditions overlap, symptoms compound each other, making treatment and daily functioning more challenging. This combination is distinct from other mood disorders like bipolar disorder or major depressive disorder, though they share some features.
In our practice, we often see clients who’ve been told they’re “just stressed” for years before receiving proper diagnosis. The relief they feel when we explain that persistent depressive disorder and anxiety are real, treatable conditions—not personal failings—is palpable. We’ve learned that helping clients understand why they experience both low mood and excessive worry simultaneously validates their struggle and opens the door to effective treatment.
The 7 Key Signs You’re Experiencing More Than Stress
1. Your “Bad Mood” Has Lasted Years, Not Weeks
Persistent depressive disorder outlasts typical sadness by months or years. While major depression might lift after several weeks of treatment, dysthymic disorder creates a depressed mood that persists for at least two years in adults or one year in children and teens.
This isn’t occasional sadness when something goes wrong. It’s feeling down, empty, or hopeless most of the day, more days than not. You might not remember the last time you felt genuinely happy. Many people with dysthymia describe it as feeling like everything is muted—not as devastating as major depressive disorder episodes, but always present in the background.
Some individuals with persistent depressive disorder experience what’s called “double depression”—periods when major depression develops on top of the chronic low mood. This layering of depressive disorders creates particularly severe symptoms that require comprehensive treatment approaches.
2. You Worry About Everything, All the Time
Excessive worry defines generalized anxiety disorder. If you constantly feel anxious about work performance, family health, finances, and everyday responsibilities—even without real threats—you might have GAD alongside dysthymia. This pattern differs from other anxiety disorders like panic disorder or social anxiety.
This worry feels uncontrollable. You know you’re overreacting, but you can’t stop your mind from spinning through worst-case scenarios. The excessive worry shifts from topic to topic throughout the day, making it hard to relax or focus.
Physical symptoms often accompany the mental distress:
- Restlessness or feeling on edge
- Fatigue that won’t quit
- Muscle tension, especially in neck and shoulders
- Difficulty sleeping or staying asleep
3. You’re Exhausted No Matter How Much You Sleep
Chronic fatigue affects both dysthymic disorder and anxiety disorders. People with persistent depressive disorder often struggle with low energy, poor appetite or overeating, and insomnia. Add generalized anxiety disorder to the mix, and your body stays in high alert mode that drains you further.
You might sleep 8 or 9 hours but still wake up tired. Or anxiety keeps you awake at night while depressive symptoms make mornings impossible. These disrupted sleep patterns create a self-reinforcing loop where fatigue worsens mood and anxiety, which then interferes with sleep quality and overall functioning.
4. Your Self-Esteem Has Hit Rock Bottom
Low self-esteem is a core feature of persistent depressive disorder and appears in the American Psychiatric Association’s diagnostic criteria. If you constantly criticize yourself, feel inadequate, or believe you’re not as capable as others, this points toward dysthymia rather than temporary stress or chronic stress alone.
This negative self-view becomes your default setting. You dismiss compliments, focus on every small mistake, or assume people secretly dislike you. When anxiety disorders co-occur, you also worry excessively about being judged or evaluated, creating additional social strain and isolation. Some personality disorders share these features, but the pattern in depression is distinct and treatable.
5. You Can’t Concentrate or Make Decisions
Difficulty concentrating affects both depressive disorders and anxiety disorders. Your mind feels foggy with depression, making it hard to think clearly or remember things. Meanwhile, anxiety fills your head with racing thoughts and excessive worry that crowd out everything else. These cognitive symptoms often mirror issues seen in other mental disorders but have specific treatment approaches.
At work or school, you might read the same paragraph multiple times without absorbing it. Simple decisions—what to eat for lunch, which task to do first—feel paralyzing. This cognitive struggle signals you’re dealing with more than everyday stress, especially when it happens consistently over months.
6. Small Tasks Feel Overwhelming
People with dysthymia often experience feelings of hopelessness that make ordinary activities feel pointless or impossibly difficult. Responding to emails, doing laundry, or returning a friend’s call can feel like climbing a mountain. This functional impairment distinguishes clinical depression from normal sadness.
Anxiety adds another layer by making you worry about doing things perfectly or fear negative outcomes. You procrastinate because starting feels too stressful, then beat yourself up for not completing tasks. This pattern of low motivation combined with excessive worry significantly interferes with daily functioning and quality of life.
7. You’ve Noticed Physical Symptoms Without Clear Medical Causes
Physical symptoms are common in both anxiety disorders and depressive disorders, affecting everything from heart rate to digestive function. Headaches, stomach problems, muscle tension, rapid heartbeat, and unexplained aches can stem from chronic depression and anxiety rather than physical illness like heart disease.
Research shows biological differences in brain chemistry for people with both conditions compared to those with only one. Your primary care doctor might rule out medical causes, but the discomfort remains. Treating mental health conditions can improve physical symptoms too.
We consistently see a pattern in our work with clients who have both conditions: they’ve often visited multiple doctors for physical complaints before anyone connected the dots to mental health. When we explain that their headaches, digestive issues, or muscle tension might be manifestations of dysthymia and anxiety—not separate medical problems—it reframes their entire understanding of their health and points toward more effective treatment approaches.
Does Dysthymia Have Anxiety?
Yes—dysthymia and anxiety frequently occur together. The combination of persistent depressive disorder and generalized anxiety disorder creates greater challenges than either condition alone. This pairing is associated with:
- Higher risk of suicidal thoughts
- More difficulty achieving full recovery
- More severe symptoms overall
- Greater difficulty with daily functioning
- Increased use of mental health services
Anxiety disorders often develop first, acting as risk factors for developing persistent depressive disorder later. Understanding that these mental health conditions frequently overlap helps explain why you might feel stuck despite trying to “think positive” or “calm down.” These are genuine mental disorders affecting brain chemistry and function, not character flaws.
What Treatment Options Actually Work?
The good news is that both depressive disorders and anxiety disorders respond well to treatment. Multiple approaches have strong evidence supporting their effectiveness.
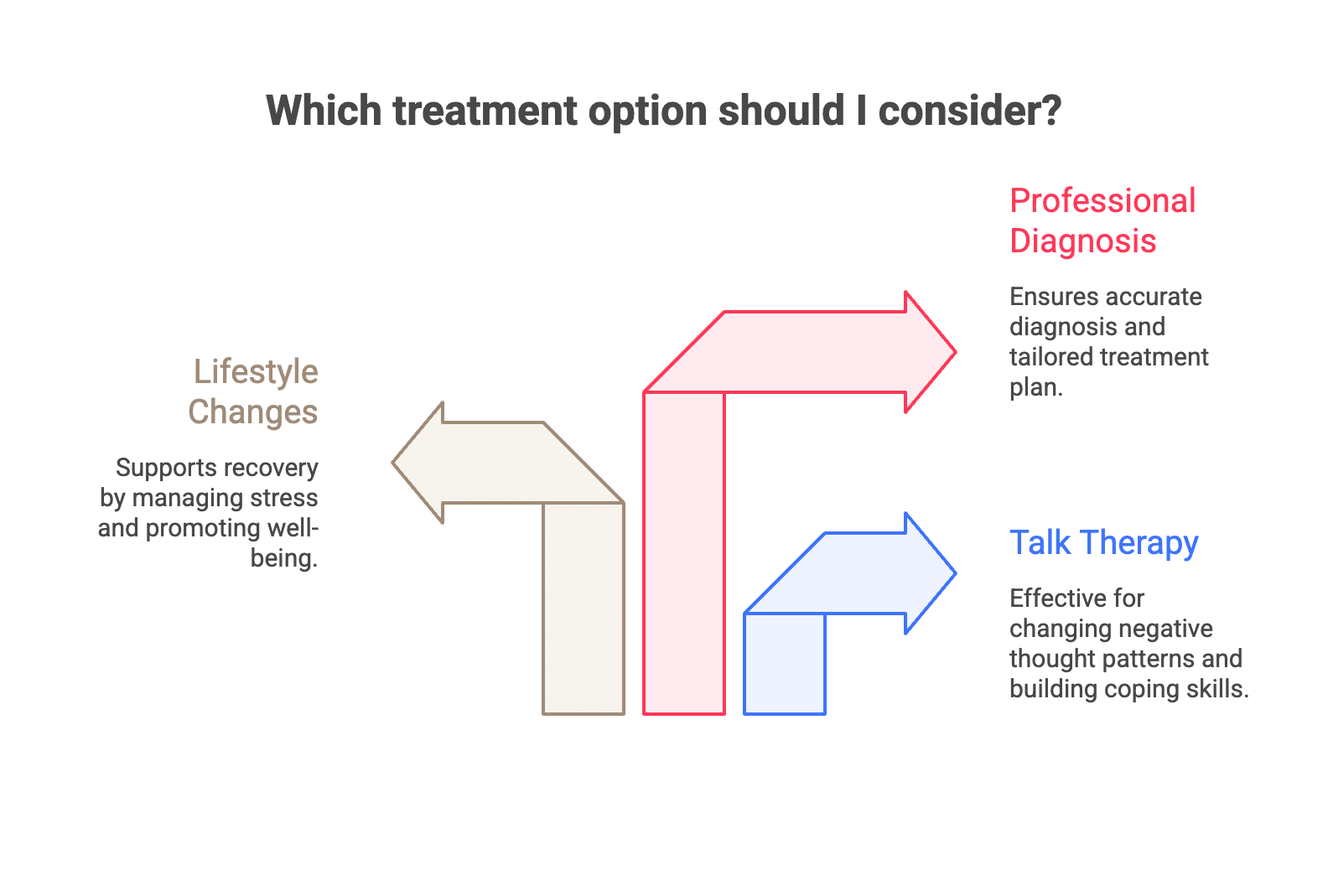
Talk Therapy
Cognitive behavioral therapy helps both depressive disorders and anxiety disorders by changing negative thought patterns and building coping skills. For persistent depressive disorder specifically, therapy addresses the deeply ingrained negative beliefs about yourself and the world. It also teaches practical strategies for managing excessive worry characteristic of generalized anxiety disorder.
Other evidence-based therapy options include interpersonal therapy, which focuses on relationship patterns, and psychodynamic approaches that explore underlying emotional patterns.
Lifestyle Changes
Lifestyle changes support recovery alongside professional treatment. Regular exercise, techniques to manage stress, mindfulness practices, and social connection all help manage symptoms of both chronic depression and generalized anxiety disorder. These strategies work as part of comprehensive treatment but shouldn’t replace professional mental health care.
Getting the Right Diagnosis
The Diagnostic and Statistical Manual provides criteria for these mental health conditions, but only a mental health professional can properly diagnose and create a treatment plan tailored to your situation. They’ll consider whether you meet criteria for persistent depressive disorder, generalized anxiety disorder, or other related disorders. Don’t try to self-diagnose—reach out for an evaluation instead.
We approach treatment for co-occurring dysthymia and anxiety by addressing both conditions simultaneously rather than treating them separately. In our experience, clients make faster progress when we help them understand how their chronic low mood and persistent worry feed into each other. We’ve found that building concrete skills for managing anxiety often gives clients enough relief to begin addressing the deeper depressive patterns that have been present for years.
How Do People with Dysthymia Behave?
People with persistent depressive disorder often appear withdrawn, pessimistic, or low-energy to others. They might:
- Cancel plans frequently due to lack of motivation
- Struggle to express enthusiasm even for activities they used to enjoy
- Have difficulty maintaining relationships due to persistent low mood
- Appear self-critical or negative in conversations
- Seem tired or overwhelmed by everyday tasks
When anxiety disorders are also present, these behaviors may combine with visible nervousness, difficulty sitting still, or excessive worry about social interactions. Understanding these behavioral patterns helps friends and family recognize when someone needs professional support rather than just “cheering up.”
What Are the Coping Skills for Dysthymia?
While professional treatment is essential for persistent depressive disorder, several coping strategies can support your recovery:
Daily structure: Creating routines helps combat the low motivation common in depression while reducing anxiety about what to do next.
Small, achievable goals: Breaking tasks into tiny steps makes them less overwhelming and provides a sense of accomplishment.
Social connection: Even brief interactions help counter isolation, a major risk factor for worsening depression.
Physical activity: Regular movement improves both depressive symptoms and anxiety, even in short 10-minute bursts.
Mindfulness practices: These techniques help manage excessive worry and reduce rumination on negative thoughts.
Sleep hygiene: Consistent sleep patterns improve both mood disorders and anxiety disorders significantly.
Remember that coping strategies work best alongside professional treatment, not as replacements. A mental health professional can teach you additional techniques through cognitive behavioral therapy or other evidence-based approaches.
Getting Help in Washington, DC
The therapists at Therapy Group of DC in Dupont Circle specialize in treating depressive disorders, anxiety disorders, and other mood disorders. Our clinicians understand the complexities of persistent depressive disorder and comorbid anxiety disorders, and can help you develop an effective treatment plan. Schedule an appointment to talk about what you’re experiencing and explore options that fit your needs.
Frequently Asked Questions about Dysthymia and Anxiety
What is depressive personality disorder and how does it relate to dysthymia?
Depressive personality disorder involves persistent patterns of self-critical, pessimistic, and gloomy thoughts that overlap with symptoms of dysthymia. While not officially classified as a separate disorder in current diagnostic manuals, it shares many features with persistent depressive disorder, especially in mood and interpersonal difficulties.
Can overeating and insomnia be symptoms of dysthymic disorder?
Yes, poor appetite or overeating and insomnia or hypersomnia are among the diagnostic criteria for persistent depressive disorder. These physical symptoms often accompany the emotional symptoms, contributing to the overall burden of the disorder.
How do genetic factors influence the development of dysthymia and anxiety?
Genetic factors play a significant role in increasing susceptibility to both dysthymia and anxiety disorders. Family history of psychiatric disorders can elevate risk, as supported by research in clinical psychology and behavioral sciences.
What role does psychodynamic therapy play in treating dysthymic patients?
Psychodynamic therapy helps patients explore unconscious emotional conflicts and early life experiences that may contribute to chronic depression. It is an evidence-based treatment option that can complement other therapies like cognitive behavioral therapy in long term treatment plans.
How is dysthymia diagnosed using tools like the Hamilton Rating Scale or self-report questionnaires?
Clinicians often use standardized tools such as the Hamilton Rating Scale for Depression and self-report measures to assess symptom severity and monitor treatment progress. These instruments help identify symptoms required for a clinical diagnosis and guide effective treatment strategies.
Are there biological differences between dysthymia and other mood disorders?
Yes, research indicates biological differences in brain chemistry and neuroendocrine function between dysthymia and other depressive disorders. These differences help explain symptom variations and inform personalized treatment approaches.
Where can I find resources from the National Institute for managing dysthymia and anxiety?
The National Institute of Mental Health provides comprehensive information on depressive disorders and anxiety, offering guidance on symptoms, risk factors, and evidence-based treatments to support individuals and families affected by these mental health conditions.
Disclaimer: This article is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or qualified mental health provider with any questions you may have regarding a medical or mental health condition. If you are in crisis or experiencing thoughts of self-harm, please call 988 (Suicide and Crisis Lifeline) or go to your nearest emergency room.