Why Is Evidence Based Practice Important in Therapy? A Plain-English Guide
What do we mean by “evidence‑based practice” in therapy?
Evidence‑based practice (EBP) means your therapist integrates three things: the best available research—including best evidence from sources like systematic reviews—their clinical expertise, and your goals, culture, and preferences. It’s not a one‑size‑fits‑all recipe; it’s a structured way to tailor care.
In plain language, EBP is a three‑part decision system that guides clinical decisions and improves clinical care and clinical practice. Therapists look at high‑quality studies and reviews, add their trained judgment about what tends to work and when, and then match all of that to you—your lived experience, identity, and what you want from therapy. This “three‑legged stool” model is the APA’s foundation for EBP in psychology (see APA’s definition of evidence‑based practice), and is closely related to the principles of evidence based medicine. When done well, it keeps therapy grounded in science and centered on the person.
- Quick example: A therapist might choose CBT skills for panic attacks because research supports them—but they’ll adjust language, pacing, and between‑session practice so it fits your culture, daily schedule, and comfort level (see a Clinical Psychology Review article on matching treatments to people). Therapists draw upon their clinical expertise and the best available knowledge to inform evidence-based practice.
Why is evidence‑based practice important for real‑world results?
EBP improves the chances you’ll feel better sooner and reduces trial‑and‑error, with better patient outcomes and improved patient outcomes as key goals.
Using proven methods tends to boost outcomes, reduce wasted time and money, and lead to lower costs. Large reviews show that therapies with strong research support help more people, more reliably and enable therapists to deliver the most effective care.
Just as important, EBP reduces blind spots: therapists commit to monitoring how you’re doing and adjusting the plan if progress stalls. The relationship still matters—a lot—but EBP helps that relationship work toward clearly defined goals, not just good vibes. This approach has a positive impact on care and brings other benefits, such as higher satisfaction and continuous quality improvement.
How does evidence‑based practice show up in a first session?
You and your therapist agree on goals, pick an approach with research support, and decide how you’ll track progress.
Here’s the simple flow most clients see:
- Clarify goals. What would “better” look like in daily life—sleeping through the night, fewer panic spikes, less conflict at home?
- Choose an approach. Your therapist proposes methods with research behind them for your concern—like CBT for anxiety, behavioral activation for depression, or EFT for couples—and explains why that choice fits your preferences and values. This selection is guided by evidence-based recommendations and informed by systematic reviews that evaluate the effectiveness of different therapeutic methods.
- Set a plan. You agree on cadence (weekly or bi‑weekly), at‑home practice, and any skills to try.
- Measure progress. This might be a brief symptom scale, a 0–10 rating of weekly stress, or tracking concrete targets like “number of nights with 7+ hours of sleep.”
- Adjust as needed. If something isn’t working, you and your therapist tweak the plan or try a different, research‑supported strategy (see an overview in Annual Review of Psychology). Evidence-based practice supports adapting patient care decisions based on ongoing evidence and your feedback.
Does evidence‑based practice make therapy “cookie‑cutter”?
No. EBP is about fit. The approach is adapted to your identity, values, and life context.
EBP doesn’t force everyone into the same script. It encourages principled flexibility: start with what the evidence says usually helps, then personalize based on culture, strengths, and feedback. This flexibility is built into structured care models, which provide a framework that can be adapted to individual needs. In practice that means we might keep the core of CBT for panic (because it works) while changing examples, metaphors, and homework so they resonate with your background and schedule.
If your feedback or the data show limited progress, EBP explicitly supports switching gears rather than doubling down on a poor fit. EBP also promotes a cohesive approach among therapists and clients, ensuring that care is both evidence-based and tailored to you.
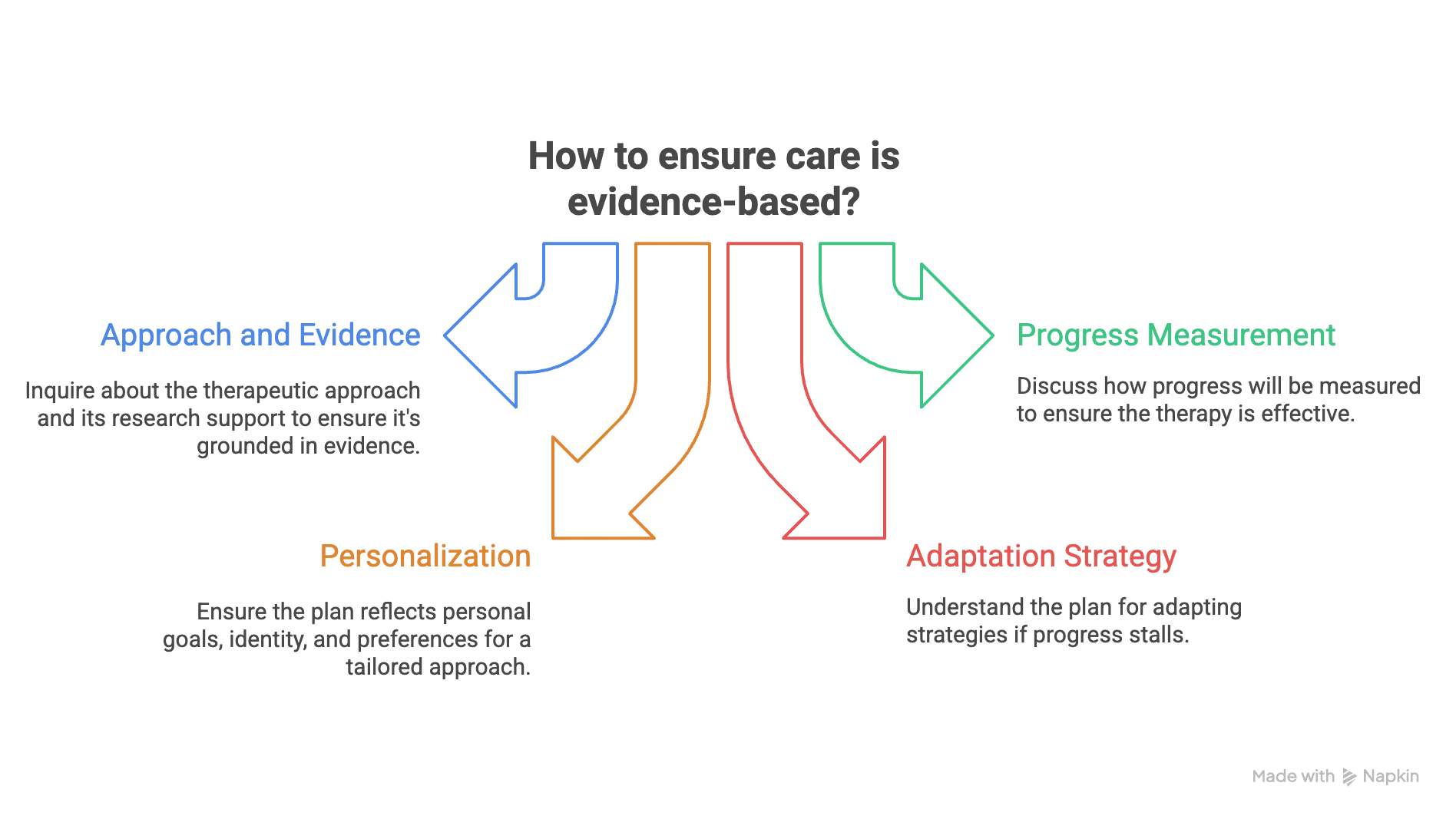
What questions can I ask to make sure my care is evidence‑based?
Ask simple, direct questions and expect clear answers.
A good therapist welcomes these kinds of questions. They show you want a plan that works and that fits your life. Asking these questions can also lead to increased confidence in the therapy process, as you become more informed and engaged in your care.
Here are four quick scripts you can use:
- “What approach are we using, and what evidence supports it?” You’re asking how research guided the choice, not for a lecture. A brief response that names the method and the evidence base is a good sign.
- “How will we know it’s helping?” Look for a concrete yardstick: fewer panic spikes, better sleep, less conflict, or a brief symptom scale you both check.
- “How will this plan reflect my goals, identity, and preferences?” EBP is a problem solving approach that includes your values and culture; the plan should show that from day one and help address your individual needs and challenges.
- “What will we change if progress stalls?” Effective care builds in decision points to adapt or switch strategies based on feedback.
How do therapists at Therapy Group of DC apply EBP in practice?
We combine research‑supported methods with a collaborative, culturally aware relationship—and we measure progress together. EBP mentors are part of our support system, guiding therapists in implementing evidence-based practice and fostering a culture of inquiry.
In Washington, DC, people are busy and stakes are high—Hill staffers, nonprofit leaders, grad students at Georgetown and GW, new parents, and long‑time Washingtonians. Our process is straightforward: agree on goals, choose a research‑supported approach, set a plan that fits your schedule, and track change in a light‑touch way, utilizing new technologies to streamline scheduling, communication, and progress tracking.
Examples include CBT for anxiety and panic, behavioral activation for depression, EFT for couples, and trauma‑informed treatments—always tailored to your culture, strengths, and comfort level. If the data or your experience say we need a different tactic, we adjust—principled flexibility over one‑size‑fits‑all.
We are committed to the further development of EBP methods and practices within our organization to continually improve care and outcomes.
Can I use a quick checklist before or after my first appointment?
Yes—use this to keep therapy focused and effective.
- Shared goals: Do we agree on 1–3 clear goals that matter in daily life?
- Supported method: Is there a named approach with evidence for my concern?
- Progress plan: Are we using a simple measure or concrete targets to see change (sleep, panic frequency, conflict episodes)?
- Fit and flexibility: Does the plan reflect my identity, values, and schedule—and do we have a plan B if needed?
What’s the simple takeaway?
Evidence‑based practice means smart, compassionate, and accountable therapy—tailored to you and guided by results.
The blend is what matters: strong research, experienced clinical judgment, and your goals and preferences working together. That combo tends to help more people more reliably—and faster—than trial‑and‑error. If you’re ready to start, make an appointment in our Dupont Circle office or via secure telehealth. We’re here to help—no pressure, just a clear plan.
Frequently Asked Questions about Evidence-Based Practice
What is the ultimate goal of evidence-based practice in nursing?
The ultimate goal of evidence-based practice (EBP) in nursing is to improve healthcare quality and patient outcomes by integrating the best available evidence, clinical expertise, and patient preferences into clinical decision making. This approach ensures high-quality patient care and optimal care outcomes.
How does evidence-based practice contribute to patient safety?
EBP enhances patient safety by promoting the use of evidence based guidelines and research findings that reduce medical errors and prevent complications. Implementing evidence based practices helps healthcare professionals make well informed decisions that prioritize patient safety in the clinical context.
What are common barriers to implementing evidence-based practice?
Common barriers include limited access to resources needed, lack of knowledgeable mentors or EBP experts, time constraints, and organizational culture that does not support or value EBP. To overcome barriers to EBP, strategies such as mentorship, targeted training, and organizational support are essential for empowering nurses and healthcare professionals to implement evidence-based practice successfully. Overcoming these barriers often requires professional development, mentorship, and a supportive healthcare system.
How do healthcare organizations benefit from implementing evidence-based practice?
Many healthcare organizations and health systems experience improved healthcare outcomes, reduced healthcare costs, and streamlined care delivery when implementing EBP. At the health system level, adopting evidence-based practices can improve efficiency, enhance patient safety, and support better overall outcomes. Embedding EBP into the culture fosters continuous quality improvement and enhances the credibility of healthcare professionals.
What role do NPD practitioners play in evidence-based practice?
Nursing Professional Development (NPD) practitioners facilitate EBP implementation by providing education, mentoring, and fostering a supportive environment. They support nursing practice by promoting evidence-based practice education and mentorship, helping healthcare professionals develop critical thinking skills and competence in the EBP process to promote positive patient outcomes.