Dating Someone with Depression: What to Know Before You Start
Dating someone with depression can feel confusing, especially if you’ve never experienced this complex mental health condition yourself. Depression affects how your partner thinks, feels, and moves through daily life. Understanding what depression looks like in a romantic relationship—and how to support your partner while protecting your own mental health—makes the difference between a healthy relationship and one that leaves both of you depleted.
Over 8.3% of adults in the United States experience at least one major depressive disorder episode each year. If you’re dating someone with depression, you’re not alone in navigating this challenge. The good news? With the right knowledge, healthy boundaries, and support, romantic relationships can absolutely thrive even when one partner lives with this mental illness.
What Is Depression and How Does It Affect Relationships?
Depression is a medical condition that affects mood, energy, motivation, and physical health. According to the World Health Organization, anxiety and depressive disorders are among the most common forms of mental illness worldwide. It’s not something your partner can simply “snap out of” or overcome with positive thinking alone. Depression often requires treatment like therapy or medication, combined with emotional support from loved ones.
In romantic relationships, depression affects how partners connect and communicate. Someone with depression may lose interest in activities they once enjoyed, including spending time together. They might experience social withdrawal, struggle with low energy, or have mood swings that feel unpredictable.
Here’s what matters: these depressive symptoms aren’t about you. They’re manifestations of mental illness, not reflections of how your partner feels about the relationship. Depression can lead to irritability, emotional instability, and unpredictability that makes it challenging to anticipate your partner’s emotional responses.
In our years working with couples navigating depression, we’ve noticed that partners often internalize withdrawal or irritability as personal rejection. One pattern we consistently see: the non-depressed partner begins monitoring every interaction for signs of “am I making it worse?” This hypervigilance actually adds stress to both people. We remind couples that depression symptoms aren’t a commentary on the relationship—they’re manifestations of an illness that’s affecting you both.
Depression affects individuals in a variety of ways. Your partner might struggle with low self-esteem, have difficulty concentrating, or feel emotionally flat even during positive moments. Understanding these patterns helps you avoid taking symptoms personally and respond with patience instead of frustration.
What Are the Signs Your Partner Is Struggling?
Recognizing depression symptoms early helps you provide better support and know when to encourage professional help. Common signs include:
- Persistent sadness or feeling emotionally numb
- Loss of interest in hobbies, socializing, or intimacy
- Changes in sleep patterns (insomnia or oversleeping)
- Low energy or fatigue, even after rest
- Difficulty concentrating or making decisions
- Social withdrawal from friends, family members, or you
- Increased irritability or mood swings
- Changes in appetite or struggle with balanced meals
Your partner’s physical and emotional needs often shift during a depressive episode. They might cancel plans frequently, need more reassurance, or have reduced libido. They may also struggle with basic tasks like maintaining routines, preparing meals, or managing responsibilities.
Being patient is especially crucial when dealing with depressive symptoms. It’s important to understand that these behaviors reflect the illness, not their commitment to the relationship. Partners who recognize this distinction report less relationship strain and better emotional capacity to provide support over time. This more accurate understanding helps you avoid frustration and maintain compassion.
How Can You Support Your Partner Without Losing Yourself?
A common mistake people make when dating someone with depression is neglecting their own mental health. You cannot pour from an empty cup, and your own well-being directly affects your ability to be a supportive partner over time.
Setting healthy boundaries protects both you and your partner’s depression from creating relationship problems. This means recognizing when you need space, maintaining friendships outside the relationship, and saying no when you’re emotionally drained or feeling overwhelmed. To set healthy boundaries isn’t selfish—it’s essential for sustainable support.
Practical ways to provide support:
- Offer specific tasks rather than vague offers (“Can I pick up groceries?” vs. “Let me know if you need anything”)
- Suggest low-pressure activities in their comfort zone, like watching a movie together or taking a short walk
- Be present without trying to “fix” their feelings
- Help create a schedule for meals, exercise, and sleep to provide a sense of control
- Encourage professional help when symptoms persist or worsen
- Practice active listening without judgment when they want to talk
- Acknowledge their progress and achievements, no matter how small
Research shows that support satisfaction matters more than the amount of support provided. Your partner benefits most when you understand what helps them specifically, rather than assuming you know what they need. Sometimes, the best support you can offer is merely being there for your partner. Consistent affection can help counteract negative feelings in a partner with depression, and physical touch can help reduce stress and anxiety in individuals with this mental health condition.
Understanding Your Partner’s Energy Levels
Monitor your partner’s energy levels to better support them day-to-day. Depression often causes low energy that makes even simple tasks feel overwhelming. Adjust your expectations based on what they can handle, and help with small daily tasks, making appointments, or planning low-stress activities when needed.
What Should You Avoid Saying or Doing?
Well-meaning advice often backfires when someone is depressed. Phrases like “just think positive” or “cheer up” minimize their struggle and can make them feel more isolated or misunderstood. These comments suggest depression is a choice or character flaw rather than a medical condition requiring professional treatment.
Avoid using unkind or derogatory language about mental health conditions, even in jest. Statements like “you’re being crazy” or “you’re too sensitive” damage trust and make your partner less likely to share their feelings with you.
Other unhelpful behaviors include:
- Taking their symptoms personally or making their depression about you
- Pushing them to socialize when they’re not ready
- Comparing their experience to someone else’s
- Offering unsolicited advice about how to manage depression
- Enabling unhealthy coping mechanisms
Instead, practice active listening and validate their feelings without agreeing with cognitive distortions or negative thoughts. You can say, “I hear that you’re feeling hopeless right now, and I’m here with you” without reinforcing distorted thinking patterns. It’s important to accept your partner’s feelings and encourage open communication about their emotional state.
When Should Your Partner Seek Professional Help?
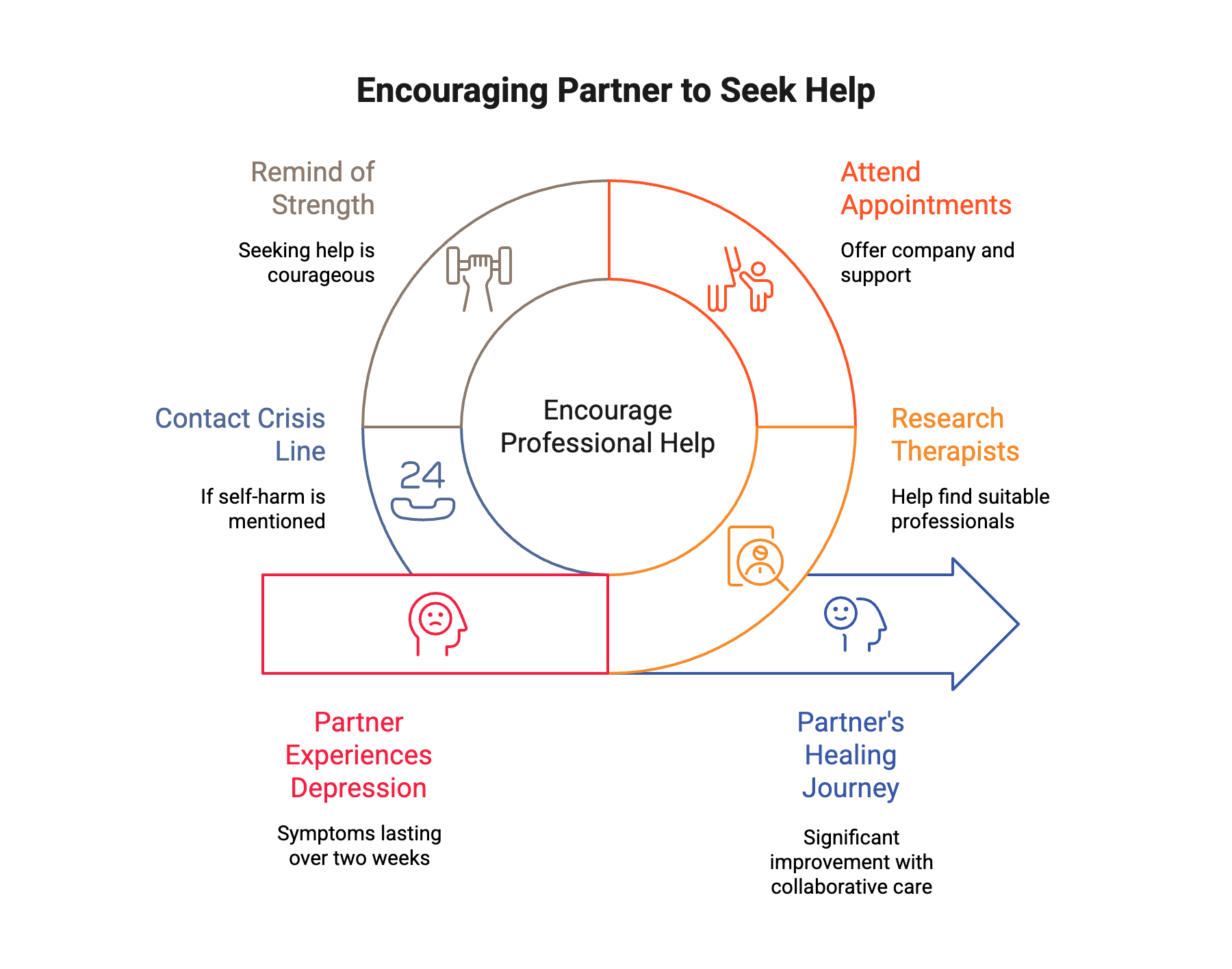
Encouraging professional help is one of the most important things you can do when dating someone with depression. Many people see significant improvement with collaborative care that combines therapy, medication when appropriate, and social support from loved ones.
Your partner should consider seeing a mental health professional if they:
- Experience symptoms lasting more than two weeks
- Struggle to complete daily tasks or responsibilities
- Have thoughts of self-harm or suicide
- Feel hopeless about the future
- Notice their depression affecting work, school, or relationships
Gently encouraging your partner to seek support shows care, not criticism. You might offer to help research therapists, attend appointments if they want company, or simply remind them that seeking help is a sign of strength. Online therapy options have made treatment more accessible for people who struggle with the energy to attend in-person sessions.
Obtaining support from friends, therapy, or support groups can be beneficial for partners dealing with this mental illness. Encouraging and assisting your partner in seeking treatment for depression can be instrumental in their healing journey. If you notice warning signs of severe depression, including talk of self-harm or suicidal thoughts, take them seriously. Don’t hesitate to contact a crisis line or seek emergency care.
How Do You Take Care of Your Own Mental Health?
Supporting a partner with depression can be emotionally draining, which is why prioritizing self-care isn’t optional—it’s essential. It is easy to become overwhelmed or neglect your own needs while focusing on supporting your partner. You cannot be a supportive partner if you’re burnt out, resentful, or struggling with your own mental health.
Taking care of your own basic needs and maintaining your social life outside the relationship helps prevent isolation. When your partner cancels plans, keep yours anyway. Spend time with friends, pursue hobbies, and engage in activities that recharge you. This isn’t abandoning your partner—it’s modeling healthy emotional awareness and balance.
Early in our work with partners of depressed clients, we thought being supportive meant endless availability and patience. Now we understand that sustainable support requires protecting your own mental health first. We often tell partners that maintaining your social life, hobbies, and boundaries isn’t abandoning your partner—it’s modeling healthy balance. The partners who thrive long-term are those who recognize they can’t be their partner’s only support system.
Consider seeking support for yourself through:
- Talking with trusted friends or family members about your experience
- Joining support groups for partners of people with mental health conditions
- Seeing your own therapist to process complex emotions and develop coping skills
- Setting boundaries around what you can realistically provide
- Practicing mindfulness or other self-care activities
- Watching educational videos to gain a deeper understanding of depression
- Seeking additional support when you’re feeling overwhelmed
Partners who access support systems report less emotional burden and greater capacity to stay present in the relationship. Support groups provide a safe space to share feelings and receive extra support from those who understand your situation. Avoiding suppressing your own emotions is important for your mental health when dating someone with depression.
Setting Boundaries for Your Own Needs
Setting healthy boundaries helps safeguard physical and emotional needs in a relationship. This is healthy for both partners in a romantic relationship where one partner has depression. Boundaries might include:
- Maintaining your own social support network
- Protecting time for self-care activities
- Being clear about your own emotional capacity
- Knowing when to seek professional guidance
- Recognizing that you can’t manage depression for your partner
Can Relationships Work When One Partner Has Depression?
Yes, absolutely. Many couples navigate depression successfully and build healthy, fulfilling relationships. The key factors that help include open communication, mutual respect, realistic expectations, and both partners taking responsibility for their mental health and well-being.
Couples therapy provides tools for communication and developing coping skills that benefit both partners. This doesn’t mean the relationship is failing—it means you’re both committed to understanding each other better and building strategies together.
What helps relationships thrive:
- Both partners understanding that depression is an illness, not a personal failing
- Clear communication about needs and boundaries
- Consistent effort from both people (even when it’s hard)
- Professional help when needed
- Patience with the unpredictable nature of depressive symptoms
- Building a more accurate understanding of how depression affects your partner
Depression doesn’t have to define your relationship, but it will require extra compassion, understanding, and intentionality from both of you. The goal isn’t to eliminate depression—it’s to build a partnership where both people feel supported, heard, and valued.
Learning More About Depression Dating
Educate yourself on depression symptoms, causes, and treatment options. This investment in learning helps you become a better support for your loved one. Resources for gaining an accurate understanding include:
- Reading articles from reputable sources about mental health conditions
- Watching educational videos about depression and relationships
- Talking to mental health professionals about how to support your partner
- Learning about depression affects relationships from trusted sources
Organizations like the National Alliance on Mental Illness (NAMI) and the National Institute of Mental Health provide essential resources for partners. Taking time to learn shows your partner you care and helps you avoid common pitfalls in depression dating.
From an attachment perspective, depression often creates what looks like a pursue-withdraw cycle in relationships. The non-depressed partner reaches out for connection, the depressed partner withdraws due to low energy or shame, which triggers more pursuing and more withdrawal. We approach this pattern by helping both partners understand that depression is driving the dance, not lack of love. Once couples see this dynamic clearly, they can interrupt it together.
Get Support in Washington, DC
If you’re in the Dupont Circle area and looking for support navigating a relationship affected by depression, the therapists at Therapy Group of DC are here to help. Schedule an appointment to get started.
Disclaimer: This article is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or qualified mental health provider with any questions you may have regarding a medical or mental health condition. If you are in crisis or experiencing thoughts of self-harm, please call 988 (Suicide and Crisis Lifeline) or go to your nearest emergency room.