Can Internal Family Systems Therapy Help with Trauma? Understanding IFS and PTSD Treatment
You’re managing a demanding career, maintaining relationships, and handling daily responsibilities—but underneath, there’s unresolved trauma that shows up in unexpected ways. Internal Family Systems therapy helps with trauma by teaching you to work with different “parts” of yourself that carry traumatic experiences, allowing healing without overwhelming your system or requiring you to relive painful events. Research shows that IFS reduces PTSD symptoms, depression, and anxiety while helping you maintain daily functioning.
What is IFS therapy and how does it work?
Internal Family Systems (IFS) therapy views your mind as made up of different “parts”—sub-personalities that hold specific feelings, beliefs, and memories. Instead of seeing conflicting thoughts or emotions as problems to fix, IFS recognizes them as protective responses that developed for good reasons, often in response to traumatic events or difficult experiences.
Richard Schwartz developed Internal Family Systems therapy in the 1980s while working with clients who described experiencing distinct parts of themselves. Rather than pathologizing this experience, Schwartz created a framework that honors these parts as a natural aspect of human psychology. The IFS model has since become particularly effective for trauma treatment because it allows you to address painful experiences without forcing direct confrontation with traumatic memories.
In IFS therapy, you work with a trained IFS therapist to identify and understand your internal system. You might notice a part that feels anxious about work performance, another part that numbs out with substance use or overworking, and still another part that holds painful memories from traumatic experiences. The goal isn’t to eliminate these parts but to help them work together more harmoniously, reducing trauma symptoms and improving your overall well-being.
IFS therapists receive specialized training through programs like those offered by the IFS Institute, learning to guide clients through the process of accessing their core Self and building healthier relationships with their parts. This training matters because working with traumatized parts requires skill in maintaining safety while addressing painful material.
The Three Types of Parts
IFS identifies three main categories of parts in your internal system:
- Exiles carry the burden of traumatic experiences and painful emotions. These parts often formed during childhood trauma or following traumatic events, holding feelings like shame, fear, or worthlessness that feel too overwhelming to face directly. They may hold memories of childhood sexual abuse, physical violence, or other experiences that exceeded your capacity to cope.
- Managers work proactively to keep you functioning and prevent exiles from overwhelming you. They might show up as perfectionism, people-pleasing, controlling behavior, or constant planning—anything to maintain mental balance and avoid triggering painful emotions. These protective parts develop sophisticated coping skills to keep you stable in daily life.
- Firefighters react when exiles get triggered and threaten to overwhelm the system. These parts use more dramatic strategies like substance abuse, binge eating, self-harm, rage, or dissociation to immediately extinguish emotional distress. While these behaviors can cause problems, understanding them as protective parts helps reduce shame.
Accessing Your Core Self
At the center of the IFS model is what Schwartz calls the “Self”—your core essence that exists separate from all your parts. When you access your Self, you experience qualities like curiosity, compassion, clarity, and calm, even when working with parts that carry intense trauma. This Self-leadership allows you to approach traumatized parts with the gentle attention they need to heal, rather than trying to fight or suppress them.
The concept of Self-leadership means your core Self can lead your internal family system with compassion and confidence. As protective parts learn to trust your Self, they become willing to step back and let you address the exiled parts carrying trauma burdens. This process gradually restores mental health and helps parts release the extreme roles they’ve taken on.
In our practice, we see how valuable IFS becomes for professionals managing demanding careers while dealing with unresolved trauma. The parts-based framework allows you to acknowledge protective patterns—like overworking or emotional detachment—without judgment, while gradually addressing the wounded parts underneath. We’ve found this approach particularly effective because it respects your need to maintain functioning while doing deeper healing work, rather than requiring intensive time off or rapid symptom increase that many high-functioning clients can’t accommodate.
How does IFS therapy help with trauma?
IFS helps with trauma by creating a safe internal relationship between your Self and the parts that carry traumatic experiences. Rather than forcing you to relive painful memories through exposure therapy techniques, IFS takes a gentle, client-paced approach where you gradually build trust with protective parts before accessing wounded exiles.
The process typically begins with getting to know your managers and firefighters—the parts that work hard to keep you safe from traumatic stress. Your therapist helps you understand what these protective parts are afraid might happen if they relax their strategies. As you develop compassion for their protective efforts, they often become willing to step back slightly, allowing access to the exiled parts carrying trauma.
When working with exiles, you maintain your grounded Self presence while witnessing what happened to these young parts. This creates a reparative experience—instead of being alone with overwhelming negative emotions, the exile receives the compassionate attention it needed originally. The part can then release the burdens it’s been carrying, updating its understanding that the trauma is over and safety exists now.
This process often improves self-esteem and self-compassion, as you learn to treat all parts of yourself with kindness rather than judgment. Many clients report better emotional regulation and fewer depressive symptoms as their internal system becomes more harmonious.
Why IFS Works for High-Functioning Trauma Survivors
Many people with trauma histories maintain successful careers and relationships while struggling internally with posttraumatic stress disorder or complex trauma symptoms. Traditional trauma therapies sometimes feel risky—taking time off work for intensive treatment isn’t always possible, and approaches that rapidly increase symptoms can feel destabilizing when you need to maintain daily responsibilities.
IFS offers a different pathway for addressing psychological trauma. Because you work with parts gradually and only access traumatized material when protective parts agree, the process respects your need for stability. You remain in control, deciding when to move deeper and when to focus on strengthening your internal system. This makes IFS particularly well-suited for professionals in demanding fields who need trauma treatment that doesn’t compromise their functioning.
IFS therapy has shown promise for addressing various mental health conditions beyond PTSD, including eating disorders, substance abuse, and other common disorders where trauma plays a role. The approach recognizes that many factors contribute to these conditions, often including experienced trauma that created protective patterns.
What are the 6 steps of IFS therapy?
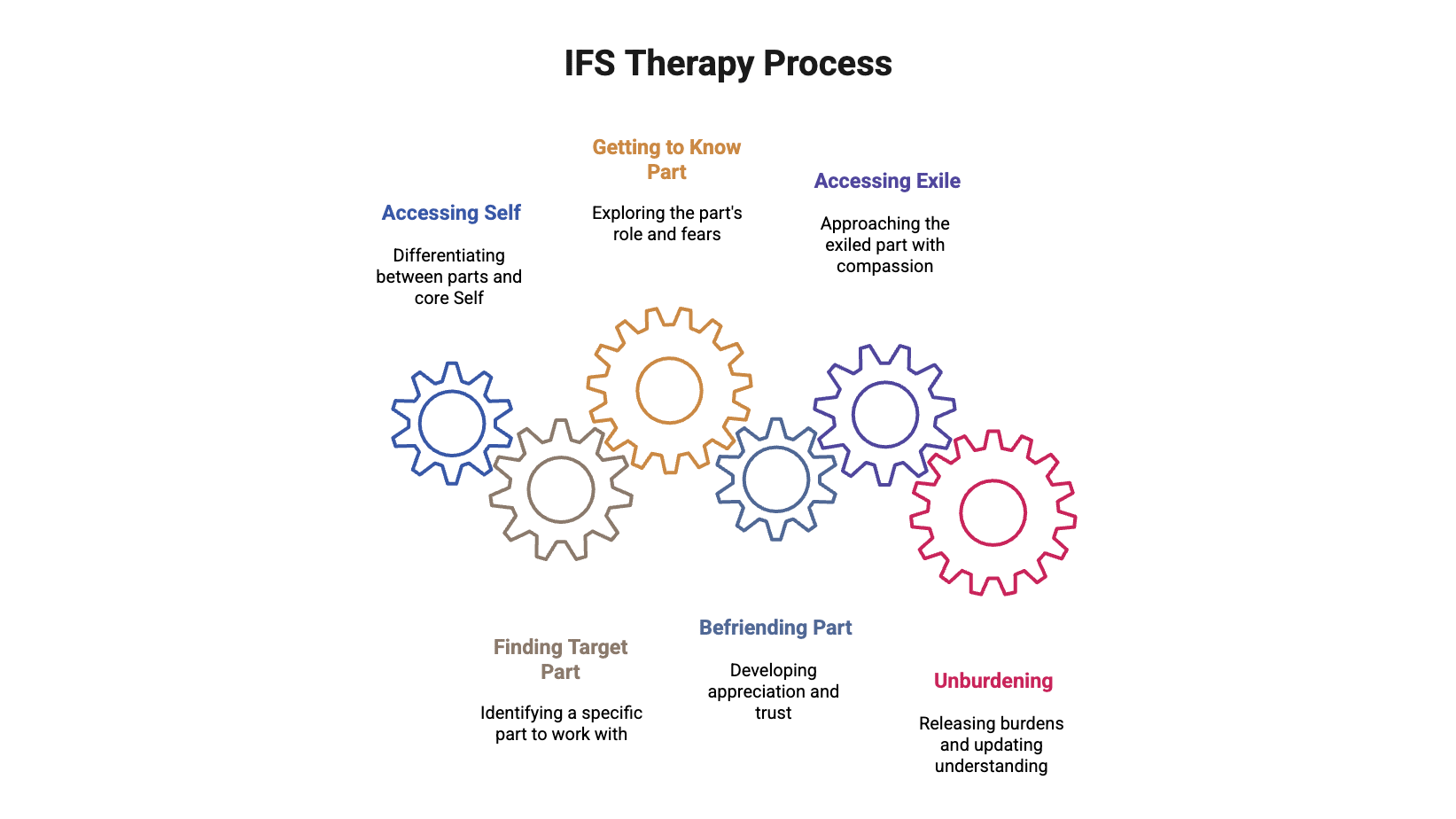
The IFS therapy process follows six main steps, though the work isn’t always linear—you might move back and forth between steps as your internal system needs:
- Accessing Self – Your therapist helps you differentiate between your parts and your core Self, learning to access that calm, curious, compassionate presence that can provide Self-leadership.
- Finding the Target Part – You identify a specific part to work with, often starting with a protective manager or firefighter causing distress in your current life, whether through substance use, self-harm, or other coping mechanisms.
- Getting to Know the Part – Through guided exploration, you learn about this part’s role, what it’s protecting you from, and what it’s afraid might happen if it stopped its protective behavior.
- Befriending the Part – You develop appreciation for the part’s efforts to protect you from traumatic stress, building trust so it might be willing to show you what it’s protecting.
- Accessing the Exile – Once protective parts trust your Self-leadership, you carefully approach the exiled part carrying trauma, witnessing its experience with compassion rather than judgment.
- Unburdening – The exile releases the beliefs and emotions it’s been holding (the “burdens” from trauma), updating its understanding that you’re safe now and the traumatic event is over.
We often tell clients who’ve tried other trauma therapies and found them too destabilizing that the six-step IFS process provides structure while remaining flexible to your pace. Some sessions might focus entirely on understanding protective parts without touching traumatic material at all, while other sessions involve deeper unburdening work—it depends on what your internal system is ready for. This pacing often makes the difference between completing treatment successfully versus abandoning therapy because it felt overwhelming.
IFS sessions can occur in individual therapy or group therapy formats, with research showing both approaches can be effective. Some IFS therapists also integrate family therapy principles when working with couples or families affected by trauma.
What is the success rate of IFS therapy?
Research on Internal Family Systems therapy shows promising results, though the evidence base is still growing compared to older trauma treatments. Studies demonstrate that IFS significantly reduces PTSD symptoms, with participants reporting decreased depression, anxiety, and improved emotional well-being. Group-based IFS programs have shown high acceptability among participants, meaning people generally find the approach helpful and manageable.
Research on IFS for depression found clinically significant improvements in a randomized controlled trial, with participants experiencing substantial symptom reduction. The approach appears particularly effective for people dealing with complex trauma—multiple traumatic experiences over time—rather than single-incident trauma. Additional randomized controlled trials are ongoing to further establish IFS effectiveness for various mental health conditions.
It’s important to understand that IFS isn’t yet considered a first-line treatment for PTSD by major clinical guidelines. The American Psychological Association’s 2025 PTSD treatment guidelines primarily recommend treatments with more extensive research backing, like prolonged exposure therapy and cognitive processing therapy. However, many mental health professionals and trauma survivors find IFS valuable, especially when other approaches haven’t worked or feel too confrontational.
What Influences Success in IFS Therapy
Several factors affect outcomes in Internal Family Systems therapy. Having a well-trained IFS therapist with sufficient training matters significantly—the approach requires specific training in the model and skill in helping clients access Self and work with parts safely. The quality of the therapeutic relationship also impacts results, as IFS requires trust to explore vulnerable internal experiences.
Your own readiness and resources matter too. IFS works best when you have some capacity to slow down and tune inward, which can be challenging during periods of crisis or overwhelming stress. Building basic emotional regulation and coping skills first sometimes helps prepare for deeper IFS work with traumatized parts.
What does trauma mean in the context of IFS?
Trauma refers to experiences that overwhelm your capacity to process and integrate what happened, leaving parts of you frozen in time carrying that unprocessed pain. In the IFS model, trauma isn’t just about the event itself but about what happens internally when a part becomes exiled because the emotions it holds feel too dangerous or overwhelming to acknowledge.
Trauma can result from obviously life-threatening experiences—physical or sexual abuse, accidents, violence, sudden loss—but also from chronic emotional neglect, betrayal, or growing up in environments where your needs couldn’t be expressed safely. What makes an experience traumatic isn’t its objective severity but whether it exceeded your capacity to cope at the time, often leaving you feeling helpless, unsafe, or fundamentally alone. If you find yourself struggling with these feelings, seeking help from a trauma therapist can be an important step toward healing.
According to the Substance Abuse and Mental Health Services Administration, trauma leads to lasting impacts on mental health and physical health conditions when left unaddressed. The effects of experiencing trauma extend beyond immediate emotional distress, potentially affecting relationships, work performance, and your sense of safety in the world.
How Trauma Creates Exiles
When traumatic experiences happen, especially involving childhood trauma or repeated traumatic events, the emotions and beliefs from those experiences get held by specific parts that become exiled from your conscious awareness. Your system essentially says, “These feelings are too much to function with, so we’ll lock them away.” Protective parts then organize around keeping those exiles buried—managers work to prevent situations that might trigger them, while firefighters stand ready to extinguish any emotional fires that break through.
This protective system works in the short term, allowing you to function and survive difficult circumstances. But over time, the effort required to keep exiles contained creates its own suffering. You might experience anxiety without knowing why, use substances or overwork to stay numb, or struggle with relationships because protective parts won’t let people close enough to trigger your exiles carrying painful emotions.
IFS addresses trauma by gently working with this protective system, helping parts understand they can relax because you now have the resources to heal those exiled wounds. The approach builds on principles from family therapy while focusing specifically on your internal family system rather than external relationships.
Getting Started with IFS Therapy in DC
If you’re experiencing trauma symptoms that interfere with your life, consider reaching out to a mental health professional trained in IFS or other evidence-based trauma treatments. Healing is possible, and you don’t have to carry these burdens alone.
Schedule an appointment with our team at Therapy Group of DC to explore whether Internal Family Systems therapy might support your healing process.
Disclaimer: This blog provides general information about Internal Family Systems therapy and trauma treatment. It is not a substitute for professional mental health advice, diagnosis, or treatment. Always seek the guidance of a qualified mental health professional with questions about your specific situation. If you’re experiencing a mental health crisis, contact the 988 Suicide & Crisis Lifeline by calling or texting 988, or seek emergency services immediately.