Evidence-Based Treatment of Depression: Talk Therapy Options in Washington, DC
If you’re experiencing depression in Washington, DC, you might be wondering about your treatment options beyond medication. Evidence-based treatment uses therapies proven effective through clinical trials, and talk therapy works just as well as antidepressants for many people—sometimes even better for preventing relapse.
Whether you’re dealing with mild depression or more severe symptoms, several proven psychotherapy approaches can help you feel better and develop lasting skills to manage your mental health. Understanding your options is the first step toward finding the right treatment for your situation.
What Is Evidence-Based Treatment of Depression?
Evidence-based treatment uses therapies with proven effectiveness through clinical trials and research studies. These aren’t just theories—they’re treatment methods validated by research showing they help people recover from major depressive disorder.
The evidence comes from multiple sources. Clinical practice guidelines from organizations like the American Psychiatric Association and the U.S. Department of Health and Human Services review thousands of clinical trials to identify which treatments actually work. These guidelines help mental health professionals make informed decisions about treating depressive disorders.
For mild depression, psychotherapy like cognitive behavioral therapy or interpersonal psychotherapy is often recommended as initial treatment. Research shows that guided self-help or a wait-and-see approach may also be appropriate for mild symptoms. For moderate or severe depression, studies demonstrate that combining medication with therapy typically produces better outcomes than either approach alone.
Depression is increasingly recognized as a major cause of disability worldwide, making access to effective treatment more important than ever. The good news? We now have more proven options than ever before for treating depressive disorders.
In our practice, we see clients surprised by how much therapy can help without medication. Many assume they need antidepressants to recover, but we’ve watched countless people find relief through therapy alone—especially when depression is mild to moderate. We approach medication as one tool among many, not an automatic first step. The research backs this up, and our clinical experience confirms it daily.
Which Talk Therapies Actually Work for Depression?
Several types of psychotherapy have strong evidence supporting their effectiveness for major depressive disorder. About half of people who try these behavioral therapies experience significant improvement in depressive symptoms, compared to about a quarter who don’t receive treatment.
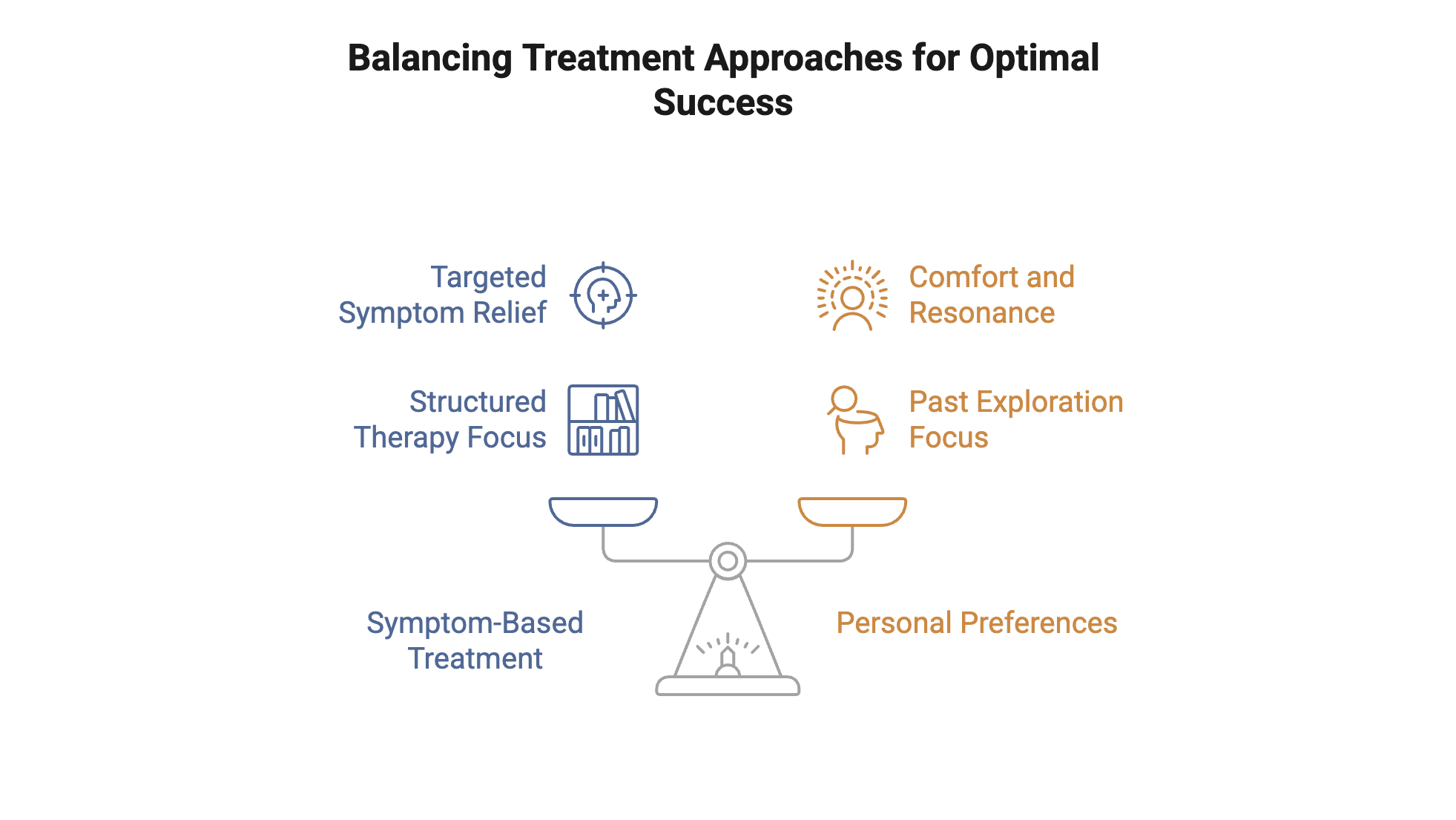
All of these approaches are considered first-line treatment options, meaning they’re recommended as initial interventions before trying other treatments. The choice between them often comes down to personal preference, symptom patterns, and what resonates with your situation.
Cognitive Behavioral Therapy (CBT)
Cognitive behavioral therapy is one of the most well-documented methods for treating depression. This approach focuses on identifying and changing negative thought patterns that contribute to depressive symptoms. If you’ve ever noticed yourself thinking “I always mess things up” or “Nothing ever goes right,” cognitive behavior therapy can help you recognize these cognitive distortions and develop more balanced, realistic ways of thinking.
Cognitive therapy typically involves 12-20 weekly sessions during the acute phase where you work with your therapist to understand how your thoughts, feelings, and behaviors are connected. The goal of acute treatment is to help you reach a remission state and return to your baseline level of functioning.
You’ll learn practical skills including:
- Behavioral activation – Gradually reintroducing pleasant activities into your life to increase positive interactions with your environment
- Cognitive restructuring – Challenging unhelpful thinking patterns and cognitive distortions
- Problem-solving therapy techniques – Managing daily challenges more effectively
Meta-analyses show that cognitive behavioral therapy is effective for reducing depressive symptoms across different severity levels. It’s particularly helpful for people who can identify specific thought patterns contributing to their depression.
Interpersonal Therapy (IPT)
Interpersonal therapy addresses how relationships affect your mood. Interpersonal psychotherapy focuses on improving problematic relationships that are linked to depression, including communication skills and resolving conflicts that may be contributing to your symptoms.
This approach is particularly helpful if your depression is connected to relationship problems, major life transitions, grief and loss, or social isolation. In Washington, DC’s fast-paced professional environment, many people find confidential therapy valuable for navigating workplace relationships and work-life balance challenges.
Interpersonal psychotherapy typically addresses four main problem areas: grief, role transitions, role disputes, and interpersonal deficits. By improving your relationships and social functioning, IPT helps reduce depressive symptoms and prevent future episodes.
Psychodynamic Therapy
Psychodynamic therapy explores how past experiences influence current emotions and relationships. Brief psychodynamic therapy typically involves 10-20 weeks of sessions focused on gaining insight into recurring patterns in your life.
Research shows that psychodynamic therapy is as effective as other evidence-based treatments for major depression. This approach can be especially valuable if you notice yourself repeating the same relationship patterns or if you want to understand the deeper roots of your depression.
Short-term psychodynamic therapy helps you understand unconscious thoughts related to your emotions and relationships, which can contribute to depressive symptoms. The therapeutic relationship itself becomes an important tool for understanding how you relate to others and yourself.
Behavioral Activation
Behavioral activation focuses on action rather than insight. The core principle is simple: doing more rewarding activities improves your mood, even when depression makes you want to withdraw from life. Behavioral activation focuses on increasing participation in positive and rewarding activities to help reduce depressive symptoms.
This evidence-based model works by reversing the cycle of depression. When you’re depressed, you tend to withdraw from activities, which leads to fewer positive experiences, which deepens the depression. Behavioral activation breaks this cycle by helping you reengage with life even before motivation returns.
Your therapist helps you identify activities that used to bring you pleasure or accomplishment, then gradually reintroduce them into your daily routine. This might mean reconnecting with friends, picking up a hobby you’ve abandoned, or simply taking walks through Dupont Circle’s tree-lined streets.
In our practice, we often see clients waiting for motivation to return before taking action. But we’ve learned that motivation follows action, not the other way around. When we introduce behavioral activation, clients are sometimes skeptical—”How can I go for a walk when I can barely get out of bed?” But what we consistently observe is that taking even small steps creates momentum. The positive experiences accumulate, and gradually clients notice their mood lifting and motivation returning naturally.
Mindfulness-Based Cognitive Therapy (MBCT)
Mindfulness-based cognitive therapy combines CBT strategies with mindfulness meditation to help you observe your thoughts without getting caught up in them. This approach integrates mindfulness practices to improve self-view and prevent relapses of depression.
Mindfulness based cognitive therapy is particularly effective at preventing depression relapse in people who’ve had multiple episodes of major depressive disorder. Research shows it’s especially helpful for those with three or more previous episodes.
This approach teaches you to notice when negative thought patterns are emerging and respond to them skillfully rather than automatically. The focus on present-moment awareness through mindfulness meditation can be especially helpful in DC’s high-stress environment where rumination and worry are common.
Acceptance and Commitment Therapy (ACT)
Acceptance and Commitment Therapy emphasizes mindfulness and values-based action rather than trying to eliminate difficult thoughts and feelings. ACT helps you cultivate psychological flexibility—the capacity to remain present and take actions aligned with your values, even when facing uncomfortable emotions.
This approach is particularly helpful if you struggle with accepting your depression or if you’ve noticed that fighting against your feelings makes them worse. ACT teaches you to observe thoughts and feelings without judgment while still taking meaningful action in your life.
Dialectical Behavior Therapy (DBT)
Dialectical Behavior Therapy addresses intense emotional regulation issues and has evidence supporting its use for depression, particularly when complicated by emotional dysregulation or suicidal thoughts. DBT combines behavioral therapies with mindfulness practices and skills training.
This comprehensive approach teaches four skill sets: mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness. While originally developed for other conditions, DBT is now recognized as an evidence-based option for treating depressive disorders when emotional instability is a significant concern.
Supportive Therapy and Supportive Psychotherapy
Supportive therapy provides a safe, empathetic relationship where you can explore your feelings and experiences. While other behavioral therapies use specific techniques, supportive therapy focuses on providing validation, encouragement, and a collaborative relationship that helps you cope effectively with stressors.
Supportive psychotherapy offers a supportive environment that enables you to explore your feelings and develop coping strategies. This approach is often used alongside other treatments or for people dealing with chronic depression who need ongoing support while managing life’s challenges.
Some psychotherapies may be more effective for people with chronic depression due to the complexity of their symptoms and the need for tailored approaches. Supportive therapy can be particularly valuable during difficult periods or life transitions.
Cognitive Behavioral Analysis System of Psychotherapy (CBASP)
CBASP is specifically designed for chronic depression. This approach combines elements from multiple therapeutic models and focuses on helping you understand how your behavior affects interpersonal outcomes. If you’ve been dealing with depression for years, CBASP may be particularly relevant.
What Makes These Treatments Evidence-Based?
The term “evidence-based” isn’t just a marketing phrase—it means these treatments have been rigorously tested in controlled research studies. Clinical trials compare people receiving specific treatments to control groups, measuring whether symptoms actually improve.
For a treatment to be considered evidence-based, it must show consistent results across multiple studies, conducted by different researchers, with diverse populations. The American Psychological Association and other professional organizations maintain registries of treatments that meet these strict criteria.
This research-backed approach matters because it helps ensure you’re investing time and energy in treatments that actually work, rather than approaches that merely sound plausible.
When Is Medication Necessary?
While this article focuses on talk therapy, understanding how medication fits into treatment can help you make informed decisions about your care.
Antidepressant Medications
Several classes of antidepressant medication have strong evidence supporting their effectiveness. Selective serotonin reuptake inhibitors, serotonin norepinephrine reuptake inhibitors, and other antidepressant classes can effectively reduce depressive symptoms for many people.
Research shows that for moderate to severe depression, combining medication with psychotherapy typically produces better outcomes than either treatment alone. The medication can help lift symptoms enough that you can engage more fully in therapy, while therapy helps you develop skills for long-term recovery.
When to Consider Medication
Your mental health provider might recommend medication if:
- You have moderate to severe depression affecting daily functioning
- You’ve tried therapy alone without sufficient improvement
- You have a history of responding well to medication
- You prefer a combined approach
- Your symptoms include significant sleep or appetite changes
For mild depression, starting with therapy alone is often appropriate. The decision should be collaborative, based on your symptoms, preferences, and circumstances.
How Do You Choose the Right Treatment?
Selecting a therapeutic approach depends on several factors including symptom patterns, personal preferences, and practical considerations.
Matching Symptoms to Treatment
Different approaches may work better for specific patterns:
- Negative thought patterns – Cognitive behavioral therapy
- Relationship difficulties – Interpersonal therapy
- Recurring life patterns – Psychodynamic therapy
- Loss of pleasure in activities – Behavioral activation
- Multiple previous episodes – Mindfulness-based cognitive therapy
- Values and acceptance issues – Acceptance and Commitment Therapy
Personal Preferences
Some people prefer structured, present-focused approaches like CBT. Others value exploring past experiences through psychodynamic therapy. Your comfort with the approach matters—therapy works better when it resonates with you.
Practical Considerations
Think about session frequency, treatment duration, and your schedule. Most evidence-based treatments involve weekly sessions for several months during the acute phase, with options for ongoing maintenance therapy.
In DC’s busy professional environment, finding a therapy schedule that works with your life is important for consistent attendance and treatment success.
The most common mistake we see is people thinking they’ve “tried therapy” when they’ve only worked with one therapist using one approach. We approach this like finding the right medication—it often takes trying different methods to find what works. A mismatch with CBT doesn’t mean therapy won’t help; it might mean IPT or psychodynamic work is a better fit. We encourage clients to think about finding the right match, not just making effort.
What About Treatment-Resistant Depression?
Some people don’t respond adequately to initial treatment attempts. Treatment-resistant depression typically means you haven’t experienced significant improvement after trying at least two different antidepressant medications at adequate doses and duration.
If standard treatments haven’t helped, several advanced options have strong evidence:
Electroconvulsive Therapy (ECT)
Electroconvulsive therapy has the highest response rates for severe, treatment-resistant depression. Modern ECT uses carefully controlled electrical stimulation under anesthesia to trigger brief seizures that can reset brain chemistry.
While ECT carries a stigma from outdated portrayals, current techniques are safe and effective. The treatment is typically reserved for severe cases that haven’t responded to other interventions, or when rapid improvement is necessary due to serious risk.
Response rates for ECT exceed those of medications or psychotherapy alone, making it a valuable option when other treatments have failed.
Transcranial Magnetic Stimulation (TMS)
Repetitive transcranial magnetic stimulation uses magnetic pulses to stimulate specific brain regions involved in mood regulation. TMS is non-invasive and doesn’t require anesthesia.
This treatment involves daily sessions over several weeks, with research showing significant improvement for many people with treatment-resistant depression. TMS has fewer side effects than medications and can be particularly valuable for people who haven’t responded to antidepressants.
Esketamine (Spravato)
Esketamine, delivered as a nasal spray in clinical settings, offers another option for treatment-resistant depression. This medication works differently than traditional antidepressants and can produce rapid improvement in some people.
Intensive Therapy Approaches
Some people benefit from more intensive therapy approaches, such as partial hospitalization programs or intensive outpatient programs that provide multiple therapy sessions per week. These programs can be particularly helpful when standard once-weekly therapy hasn’t produced sufficient improvement.
What Happens After Treatment?
Recovery from depression requires ongoing attention even after symptoms improve. Understanding maintenance strategies helps prevent relapse and sustain progress.
Continuation and Maintenance Therapy
After reaching remission, many people benefit from continuation therapy—ongoing sessions at reduced frequency to consolidate gains and prevent relapse. Research shows that continuing therapy after symptom improvement significantly reduces the risk of depression returning.
Maintenance therapy might involve monthly check-ins or sessions scheduled as needed during stressful periods. This ongoing support helps you apply skills learned in therapy and catch early warning signs before they develop into full episodes.
Booster Sessions
Even after completing therapy, periodic booster sessions can refresh skills and provide support during challenging times. Many people find that occasional check-ins help them stay on track and address emerging concerns before they escalate.
Lifestyle Factors
Several lifestyle elements support ongoing mood stability:
- Physical exercise – Regular activity improves mood and reduces depressive symptoms
- Sleep hygiene – Maintaining consistent sleep patterns supports mood regulation
- Nutrition – A balanced diet supports both physical and mental health
- Social connection – Maintaining relationships combats isolation
Stress Management
Learning to manage stress reduces vulnerability to depression relapse. This might include:
- Setting realistic boundaries at work and home
- Practicing relaxation techniques
- Balancing responsibilities with self-care
- Identifying and reducing unnecessary stressors
Support Systems
While therapy provides professional support, personal connections matter too. Family and friends can offer encouragement, practical help, and emotional support throughout your recovery.
Common Questions About Evidence-Based Treatment
What is proven to be the most successful treatment for depression?
No single treatment is “most successful” for everyone. For mild depression, psychotherapy alone is often effective. For moderate to severe depression, combining antidepressant medication with psychotherapy typically produces the best outcomes. For treatment resistant depression, electroconvulsive therapy has the highest response rates.
The most successful approach for you depends on your specific symptoms, preferences, and circumstances.
Which of the following is an evidence-based treatment for depression?
Evidence-based treatments include cognitive behavioral therapy, interpersonal psychotherapy, psychodynamic therapy, behavioral activation, mindfulness based cognitive therapy, and several other psychotherapeutic interventions. For medications, selective serotonin reuptake inhibitors, serotonin norepinephrine reuptake inhibitors, and other antidepressant classes have strong evidence. Advanced options like electroconvulsive therapy and repetitive transcranial magnetic stimulation also have robust research support.
What are some examples of evidence-based treatment?
Examples include:
- Cognitive behavioral therapy and its variations
- Interpersonal therapy for depression
- Brief psychodynamic therapy
- Behavioral activation
- Mindfulness based cognitive therapy
- Acceptance and Commitment Therapy
- Dialectical Behavior Therapy
- Problem solving therapy
- Cognitive Behavioral Analysis System of Psychotherapy for chronic depression
All of these have demonstrated effectiveness in multiple clinical trials and are recommended in clinical practice guidelines from major health organizations.
How do I know if I need medication or therapy alone?
Treatment selection depends on several factors including symptom severity, functional impairment, and personal preferences. For mild depression, therapy alone is often sufficient. For moderate symptoms, either approach or a combination may be recommended. For severe depression, combination treatment with both medication and therapy typically works best.
Your mental health provider can help assess your symptoms and discuss options. Some people prefer to try therapy first before adding medication, while others benefit from starting both simultaneously.
Moving Forward with Treatment
Depression is treatable and many people recover with the right support and treatment. While progress isn’t always linear—setbacks happen and recovery takes time—effective help is available.
The most important first step is reaching out. Whether you choose cognitive behavioral therapy, interpersonal psychotherapy, psychodynamic therapy, or another evidence-based approach, starting treatment moves you toward feeling better.
Research continues to expand our understanding of depression and develop new treatments. The evidence base grows stronger each year, offering hope that we can help more people find relief from depressive symptoms and build fulfilling lives.
Getting Started with Evidence-Based Depression Treatment in DC
If you’re looking for evidence-based treatment of depression in Washington, DC, the therapists at Therapy Group of DC are here to help. We offer out-of-network talk therapy using proven approaches including cognitive behavioral therapy, interpersonal psychotherapy, psychodynamic therapy, behavioral activation, mindfulness-based approaches, and other evidence-based methods tailored to your needs.
Our therapists in Dupont Circle understand the unique pressures of living and working in DC and can help you find the right therapeutic approach for your situation. Schedule an appointment to get started.
Disclaimer: This article is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or qualified mental health provider with any questions you may have regarding a medical or mental health condition. If you are in crisis or experiencing thoughts of self-harm, please call 988 (Suicide and Crisis Lifeline) or go to your nearest emergency room.