The 5 R’s of Depression: Evidence-Based Coping Tools for Depression
Feeling overwhelmed by depression can make it hard to know where to start with coping strategies. Research shows that combining multiple approaches leads to better outcomes than relying on just one coping tool. Evidence from clinical practice demonstrates that addressing different aspects of depression simultaneously—your physical health, relationships, daily routines, and access to professional support—creates the most effective path to alleviating depression and improving well-being.
The 5 R’s of depression offer a practical framework for recovery: Rest, Relationships, Routine, Recreation, and Resources. Each category includes specific coping strategies backed by evidence from psychiatry and mental health research. Understanding these five areas can help you build a personalized approach to managing depressive symptoms and reducing stress in your life.
What Are the 5 R’s of Depression?
The 5 R’s are five categories of coping strategies that target different aspects of depression recovery. They include Rest (sleep and stress management), Relationships (social support), Routine (daily structure), Recreation (enjoyable activities and exercise), and Resources (professional help). This framework helps organize the many evidence-based approaches into manageable groups that address how depression affects your mood, thinking, and daily life.
Mental health professionals use this framework in clinical practice because depression affects multiple areas of life simultaneously. Physical exercise improves mood and reduces symptoms, while social support buffers against negative emotions. By addressing all five areas, you create a comprehensive coping strategy rather than relying on a single approach. This matters because research consistently shows that people who practice multiple coping strategies experience greater improvement in depressive symptoms than those who focus on just one area.
The 5 R’s work because they acknowledge that depression isn’t just about feeling sad—it affects your sleep, relationships, daily habits, ability to focus, and capacity to experience positive emotions.
1. Rest: Supporting Your Body’s Foundation
Adequate sleep and stress reduction form the foundation of depression recovery. When you’re depressed, sleep disturbances are common—either sleeping too much or struggling with insomnia. Research shows that addressing sleep patterns helps stabilize mood and improves your ability to cope with daily challenges and stress.
Rest doesn’t only mean sleeping. Staying away from stressors provides necessary space for self-healing, giving your nervous system time to regulate and your mind a few seconds to process emotions without pressure. This might mean:
- Setting boundaries at work or with demanding relationships to reduce workplace stress
- Limiting exposure to stressful news or social media that triggers anxious thoughts
- Saying no to obligations that drain your energy and affect your well-being
Practice good sleep hygiene by maintaining consistent sleeping patterns, avoiding screens before bed, and creating a calm environment. If anxiety keeps you awake, mindfulness techniques like the 5-4-3-2-1 grounding method can help you focus on the present moment rather than racing thoughts. Practicing mindfulness involves observing feelings without judgment, which can mitigate anxiety and panic that often accompany depression.
Eating a balanced diet rich in whole foods can improve mental and emotional health by supporting your body’s ability to regulate mood and manage stress.
In our practice, we’ve noticed that clients often feel guilty about resting, as if they should be “doing more” to fight depression. We remind them that depression is exhausting—it takes enormous energy just to get through the day with this weight. Rest isn’t giving up or being lazy; it’s recognizing that your brain and body need recovery time. We’ve seen clients make more progress after they stopped pushing themselves relentlessly and started honoring their need for genuine rest. Sometimes the most productive thing you can do is nothing at all.
2. Relationships: The Power of Social Support
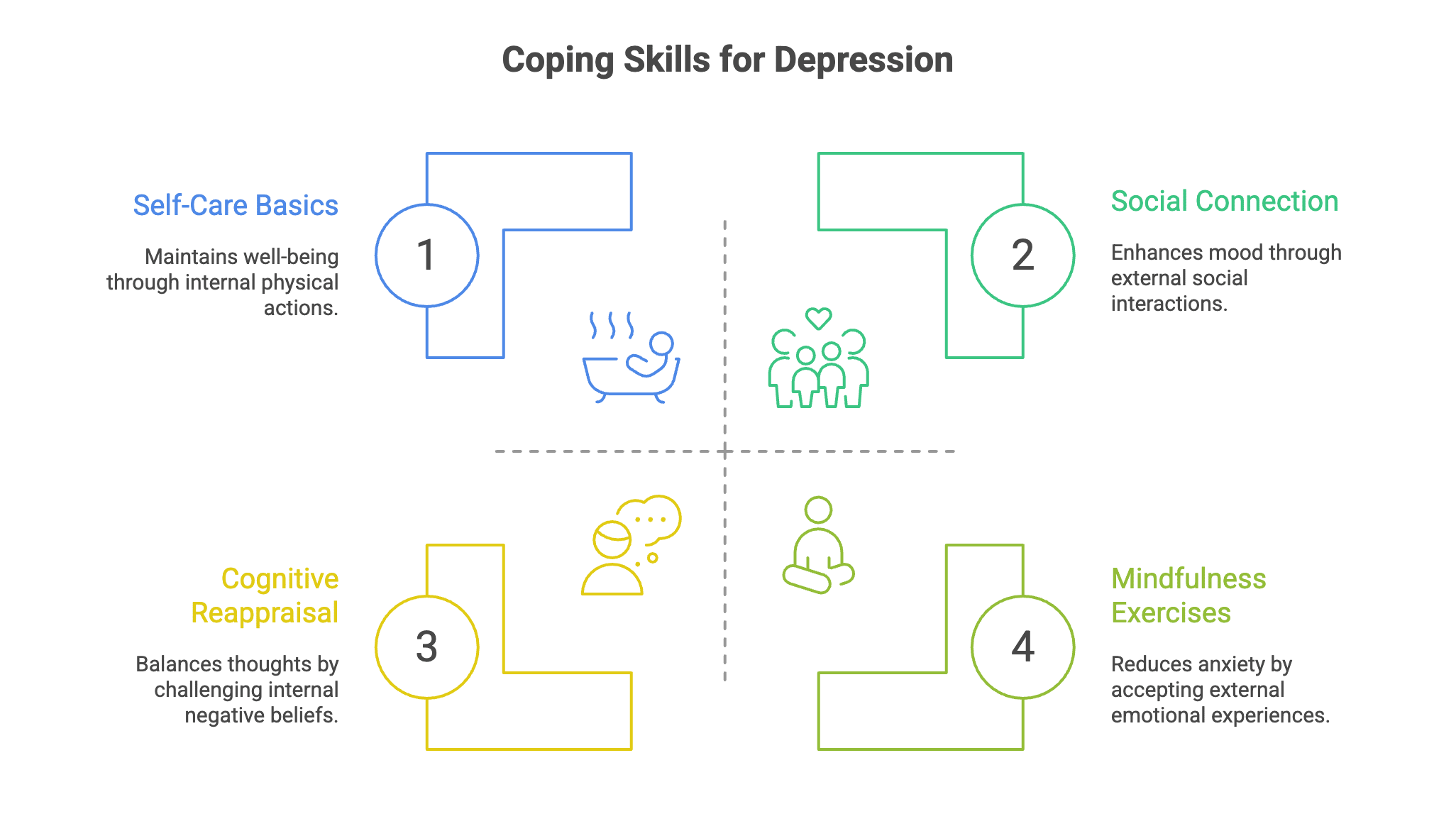
Connecting with trusted friends or family significantly buffers the negative impact of depression on your well-being. Even when you feel like isolating yourself, maintaining relationships is one of the most effective coping strategies for depression available. Research shows that social support enhances self-esteem, confidence, and your sense that you can handle life’s challenges. Both family and peer support are identified as crucial sources of interpersonal support for individuals suffering from depression.
Reaching out doesn’t mean you need to explain everything you’re feeling. Sometimes just being around others—grabbing coffee with a friend in Dupont Circle or calling a family member—can improve your mood. Peer support networks offer empathy from people who share similar experiences, which reduces feelings of isolation and provides a non-judgmental space for dealing with depression.
Here’s why social connection matters for coping with depression:
- Volunteering or helping others creates a sense of value and purpose that combats feelings of emptiness
- Talking to others about feelings provides relief from depression and improves mental well-being
- Simply being around supportive people lifts your mood and enhances positive emotions, even when you don’t initially feel like participating
- Interactions with others who have similar experiences lead to greater empathy and understanding, enhancing feelings of connection
Maintaining relationships despite feelings of isolation is critical for alleviating depression. You don’t have to go through this alone. Opening up to people you trust often provides relief while strengthening your connections with those who care about you.
3. Routine: Creating Structure When Life Feels Chaotic
Maintaining a daily routine supports emotional health by providing predictability and purpose when depression disrupts your sense of structure. You might skip meals, lose interest in eating, let hygiene slide, or lose track of time. Building even a simple routine helps counter these effects and reduces the feeling of being controlled by depression.
Start small by identifying a few anchors for your day. This could be eating regular meals at the same time, taking a short walk each morning, or getting dressed even when staying home. Breaking big problems into smaller, manageable steps makes them feel less overwhelming, gives you a sense of control, and helps you develop sustainable coping strategies over time.
Keep track of your mood and activities in a journal. Research shows that keeping a journal of emotions can improve self-regulation and understanding of one’s feelings. Writing down your emotions and what you do each day helps you notice patterns—you might discover that certain activities consistently improve your mood, or that specific times of day present greater difficulty or challenges. This awareness allows you to plan coping strategies more effectively for your unique situation.
Members of online depression communities describe self-reflection through journaling as a way to understand their emotional states better. Set achievable goals and celebrate progress, no matter how small. Getting out of bed, taking a shower, or completing one task counts as a win when you’re dealing with depression.
4. Recreation: Finding Moments of Enjoyment
Engaging in recreational activities and physical exercise reduces negative emotions and alleviates anxiety. Even when you don’t feel like participating, activities that once brought you joy can help lift your mood and affect your overall mental health positively. The key is starting small and not pressuring yourself to feel immediate happiness.
Physical exercise doesn’t have to be intense to benefit your mental health. Walking for just 20 minutes every day can improve your well-being and serve as a good starting point for building an active lifestyle. Exercise effectively stimulates the central nervous system and alleviates symptoms of depression by inhibiting the breeding of negative emotions and increasing positive emotions. Participating in physical activities can distract attention from negative thoughts and improve mood.
Ways to add recreation and exercise to your routine:
- Join a group exercise class to benefit from both movement and social interaction, which further enhances mood
- Spend time outdoors walking in DC’s parks and green spaces
- Listen to music, read, or pursue creative hobbies that provide a sense of interest and engagement
- Schedule pleasant or relaxing activities intentionally, like any other important matter in your life
People who engage in regular physical activity report feeling happier than those who do not. Research demonstrates that exercising regularly can help prevent depression from returning after recovery. The goal isn’t to force yourself to feel joy immediately—think of recreation as planting seeds that gradually shift your emotional state and perspectives over time.
You don’t have to enjoy an activity in the moment for it to help your depression. We see clients who make themselves to go to yoga or meet a friend for coffee while feeling nothing—and then notice their mood is slightly better an hour later. The benefit isn’t always immediate or obvious. We encourage clients to think of pleasant activities as medicine you take whether you feel like it or not, trusting the delayed effect.
5. Resources: Seeking Professional Support
Professional help plays a significant role in the rehabilitation of depression, especially when symptoms persist for more than two weeks. While self-management coping strategies are valuable, they work best when combined with evidence-based treatment. Seeking professional support is one of the most important coping tools for depression you can use, particularly when dealing with significant symptoms that affect your daily life, work, and relationships.
Therapies like Cognitive Behavioral Therapy and Interpersonal Therapy help you identify and change negative thought patterns that fuel depression and negative thoughts. In simple terms, CBT gives you tools to challenge harsh self-talk, reframe situations, and develop healthier thinking strategies. Dialectical Behavior Therapy (DBT) can also be effective in treating depression by teaching skills for emotion regulation and distress tolerance.
You can refer yourself for talking therapies like cognitive behavioral therapy or counseling—you don’t always need a referral from your doctor to begin the process of getting help.
Local resources in DC can help you get started:
- The ACCESS Helpline is the primary resource for connecting to mental health services in DC
- Federally Qualified Health Centers (FQHCs) provide affordable mental healthcare services
- Urgent Care Clinics offer same-day assessment, counseling, and psychiatric evaluations
- NAMI DC provides education, support, and advocacy for individuals and families affected by mental illness
If you’re still feeling down or depressed after a couple of weeks of trying coping strategies, get professional help. Treatments for depression include talking therapies and antidepressants, and your healthcare provider can explain different options based on your specific symptoms and situation. If you’re struggling with side effects from treatment or not feeling better, talk openly with your provider about other options. Treatment effectiveness varies by person, and finding the right approach sometimes requires adjustments.
What Are Some Good Coping Skills for Depression?
The most effective coping skills address both thoughts and behaviors through a combination of self-management strategies and professional support. Research in clinical practice consistently shows that mixing strategies—like combining exercise with therapy, or adding social connection to stress reduction—produces better outcomes and greater improvement in mood than any single approach to alleviating depression.
Helpful thinking strategies include noticing negative thoughts and challenging them. When you catch yourself thinking “I’m worthless” or “Nothing will ever get better,” ask yourself if there’s another perspective on the situation. Replace harsh self-talk with kinder, more realistic thoughts. This form of cognitive reappraisal doesn’t mean forcing positive thinking—it means finding a balanced perspective. Stopping self-blame reduces negative emotions and helps you reappraise difficult situations more accurately.
Mindfulness and relaxation exercises help you accept difficult feelings without judgment, reducing the anxiety and panic that often accompany depression. Self-reconciliation includes perceiving feelings, accepting the present self, and holding hope for the future. Practicing self-acceptance—perceiving and accepting your feelings rather than fighting them—can help reduce anxiety and panic caused by emotional uncertainty.
Building your own standards and values helps eliminate feelings of being controlled by others and gives you a sense of agency in your recovery process. Self-care basics matter more than you might think. Taking a shower, getting dressed, eating regular food, and spending time outdoors all support your mental health. These simple actions maintain your physical health, which directly affects your emotional well-being and ability to cope with stress.
How Do I Build My Own Depression Coping Toolkit?
Start by choosing one strategy from each of the 5 R’s and practicing consistently before adding more. Trying to implement everything at once usually leads to feeling overwhelmed and increases the risk of giving up. Instead, build your toolkit gradually based on what resonates with you and fits your life circumstances.
Experiment with different approaches to see what helps your specific symptoms and situation. Some people find exercise transformative for their mood, while others benefit most from social support or talk therapy. Your toolkit should reflect your preferences, lifestyle, and specific depressive symptoms. What works for someone else might not work for you, and that’s okay—finding ways to cope that fit your life is what matters.
Track what you try and how it affects your mood and well-being. This helps you identify which coping strategies deserve a permanent place in your toolkit and develop confidence in your ability to manage depression. If something isn’t helping after giving it a fair chance, let it go and try something else. Research shows this process of examining different approaches helps people find the most effective combination of coping tools.
Here’s why this matters: Depression recovery isn’t one-size-fits-all, and what helps during one phase of recovery might differ from what you need later. Working with a therapist helps you refine your approach, provides accountability as you build new habits, and offers professional perspective on your progress. Combining self-management with professional support typically produces the best outcomes and supports long-term recovery.
When Should I Seek Professional Help?
If symptoms persist for more than two weeks, interfere with daily life, or include thoughts of self-harm, seek professional help immediately. Professional treatment isn’t a last resort—it’s one of the most effective coping strategies available and often makes other self-management tools work better by providing structure, evidence-based techniques, and support through the recovery process.
Warning signs that it’s time to reach out for professional support include:
- Persistent sadness, emptiness, or depressed mood most of the day
- Loss of interest in activities you once enjoyed
- Difficulty concentrating, making decisions, or dealing with daily challenges
- Changes in appetite or eating patterns
- Significant changes in sleeping habits (insomnia or sleeping too much)
- Fatigue, low energy, or feeling slowed down
- Feelings of worthlessness, excessive guilt, or suffering
- Thoughts of death or suicide
Seeing a doctor or mental health professional plays an important role in the diagnosis and treatment of depression. They can examine your symptoms, rule out other medical conditions, and recommend evidence-based treatments tailored to your situation.
If you’re in crisis or experiencing thoughts of self-harm, don’t wait. Call 988 (Suicide and Crisis Lifeline) for immediate, confidential support, or go to your nearest emergency room. Immediate support is available 24/7, and reaching out is the first step toward getting the help you need.
From a clinical perspective, we’ve observed that clients often see seeking help as admitting defeat—as if they should be able to handle depression alone. We approach this differently in our practice. We tell clients that reaching out for professional support is actually one of the most effective coping strategies available, not a last resort. The clients who combine self-management with therapy typically make faster progress and develop stronger skills than those who try to do everything alone. Seeking help isn’t weakness; it’s recognizing that depression is a serious condition that responds best to comprehensive treatment.
Ready to Get Started?
You don’t need to handle depression alone. The therapists at Therapy Group of DC in Dupont Circle specialize in evidence-based treatments that help you develop effective coping strategies tailored to your situation. Whether you’re suffering from persistent depressive symptoms, difficulty with relationships, or challenges maintaining your daily routine, professional support can help. Schedule an appointment to start building your path toward recovery and improved well-being.
Disclaimer: This article is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or qualified mental health provider with any questions you may have regarding a medical or mental health condition. If you are in crisis or experiencing thoughts of self-harm, please call 988 (Suicide and Crisis Lifeline) or go to your nearest emergency room.