Depression After a Breakup: When Heartbreak Becomes Depression
Breaking up with someone hurts. You might feel sad, angry, confused, or completely lost—and that’s completely normal. But sometimes, the pain goes deeper than expected sadness. Depression after a breakup is real, common, and different from the normal grief that follows the end of a relationship.
Understanding when heartbreak crosses into depression can help you recognize if you need additional support. Let’s explore the difference between normal post-breakup grief and clinical depression, and what steps to take if you’re struggling with your mental health after a romantic relationship breakup.
What’s the Difference Between Normal Sadness and Depression After a Breakup?
Normal sadness shifts and lessens over time, while depression tends to feel stuck and pervasive. When a romantic breakup happens, feeling sad is one of the most common human responses to loss. You’re grieving not just the person, but the future you imagined, the routines you shared, and sometimes even parts of your self concept.
Stressful life events like breakups can trigger emotional distress, and for many people, these feelings gradually improve with time and social support. Normal sadness might include crying, missing your former partner, feeling lonely, or questioning your decisions. These feelings usually come in waves—intense one moment, manageable the next. You might feel sad one day but find yourself laughing with friends the next.
Major depression feels different. Depression involves persistent symptoms that affect all aspects of your life and don’t lift after a few days or weeks. According to the DSM-5, major depressive disorder requires at least five specific symptoms lasting at least two weeks and significantly interfering with daily functioning.
In our practice, we use what we call the “wave test” with clients struggling after breakups. We ask: “When something good happens—a friend texts, you see a funny video, you get good news—can you feel anything positive, even briefly?” With normal grief, the answer is usually yes, even if the positive feeling fades quickly. With depression, clients often say they feel nothing, or the good moment gets immediately swallowed by emptiness. That inability to experience even brief moments of relief is often the clearest signal that we’re dealing with depression rather than normal heartbreak.
What Are the Symptoms of Depression After a Breakup?
Depression changes how you think, feel, and function—it’s more than just feeling sad. Research shows that emotional responses to a breakup often resemble symptoms of clinical depression. Here’s what depressive symptoms can look like when a relationship ends:
Emotional symptoms:
- Persistent sadness, emptiness, or hopelessness that doesn’t lift
- Loss of interest in activities you normally enjoy
- Feelings of worthlessness or excessive guilt
- Increased irritability, anger, or frustration
- Suicidal thoughts or suicidal ideation
Physical symptoms:
- Sleep problems—insomnia or sleeping too much
- Appetite changes and significant weight shifts
- Fatigue or loss of energy every day
- Physical aches without clear cause
Cognitive symptoms:
- Difficulty concentrating or making decisions
- Memory problems
- Negative feelings that loop repeatedly
- Feel confused about who you are without the relationship
If you’re experiencing five or more of these symptoms most of the day, nearly every day for at least two weeks, and they’re making it hard to function at work, school, or in other relationships, you may be dealing with major depression rather than normal sadness. Depression can lead to prolonged feelings of apathy and significant impairment in areas of life functioning.
Can a Breakup Really Cause Depression?
Yes—romantic breakups are among the most stressful life events people experience, particularly during emerging adulthood. Research shows that unmarried relationship dissolution can trigger depressive symptoms in many individuals, though not everyone who goes through a romantic breakup develops depression.
Several risk factors make someone more vulnerable to depression after major life changes:
Attachment-related factors: People with attachment anxiety—characterized by negative self-image, excessive doubts about self-worth, and fear of abandonment—are more likely to experience elevated depressive symptoms after the end of a romantic relationship. These individuals often struggle more with self-concept and self esteem following a breakup. Research indicates that pre-breakup attachment insecurities are related to higher post-breakup depressive and anxiety symptoms through maladaptive coping strategies like self-punishment.
Studies show that individuals with high levels of attachment anxiety tend to use maladaptive coping strategies, which can explain their increased breakup distress. Attachment avoidance is also related to less use of accommodation coping and can lead to greater depressive symptoms post-breakup.
Pre-existing vulnerabilities: If you’ve experienced major depression before, had a history of trauma, or have limited family and friend support, you face higher risk for depression after major life events. The adjustment period after a breakup can involve profound feelings of distress and loss, particularly if you’re also dealing with other stress in your life.
Circumstances of the breakup: Breakups involving intimate partner violence, betrayal, or unexpected abandonment can be particularly devastating to mental health and well being. The way a relationship ends matters significantly for emotional recovery.
Life context: University students and young adults going through breakups often face additional challenges during emerging adulthood. The end of a relationship can affect academic performance, life satisfaction, and your sense of identity during an already unstable time. Research has found that breakups can influence self-esteem and academic performance negatively, especially when you’re still figuring out who you are as a person.
We often tell clients that sometimes the breakup doesn’t directly cause depression—instead, the relationship may have been masking underlying mental health issues. We’ve worked with people who functioned well while partnered because their partner provided structure, validation, or distraction. When the relationship ended, issues with self-worth, anxiety, or depression that were always present suddenly became impossible to ignore. Many individuals may feel insecure in their self-image following a breakup, and that’s actually when the real healing work can begin.
How Long Does Depression Last After a Breakup?
There’s no universal timeline for the healing process—recovery depends on many individual factors. Normal sadness after a romantic relationship ends usually begins to lift within a few weeks to a couple of months as you adjust to your new life.
Depression follows a different pattern. Adjustment disorder—a stress-related condition that can develop after stressful life events—typically improves within six months once you’ve adapted to the change. Adjustment disorder involves clinically significant emotional or behavioral symptoms in response to a major life event like a breakup. If depressive symptoms persist beyond six months or significantly impair your functioning, it may indicate major depression requiring professional help from a mental health professional.
The healing process isn’t linear. You might have good days followed by difficult ones, especially around reminders of your ex-partner or significant dates like anniversaries. This is completely normal. What matters is whether you’re seeing overall improvement over weeks and months, not day to day.
Research on emerging adulthood suggests that coping strategies significantly influence how long depression lasts after a breakup. People who use healthy coping mechanisms tend to recover faster than those who rely on maladaptive strategies like self-punishment, substance use, or complete withdrawal from friends and family.
Over time, emotional responses to a breakup usually begin to shift as individuals heal and recover. For some, feelings following a breakup can lead to prolonged emotional distress, which may require additional support or intervention from a clinical psychologist or therapist.
What Is the 3-Week Rule for Breakups?
Some people refer to a “3-week rule” suggesting it takes about three weeks to start feeling better after a breakup. This isn’t a scientific timeline—everyone’s healing process is different. While you might notice some emotional shifts after a few weeks, true healing takes longer.
If depressive symptoms persist or worsen after two to three weeks, it’s important to seek professional help rather than waiting for an arbitrary timeline to pass. Trust your own experience and reach out for support when you need it.
What Coping Strategies Actually Help With Depression After a Breakup?
The strategies you use can either help or hinder your emotional recovery. Research shows that the coping strategies employed by anxiously attached individuals can increase their breakup distress over time. Here’s what research and clinical experience tell us about healthy ways to cope:
Healthy Coping Strategies That Work
Reach out for social support. Talk to friends and family members about your feelings and emotions. Surrounding yourself with supportive people validates your experience and reminds you that you’re not alone. Connecting with supportive friends and family can provide essential emotional support during difficult times. If your social circle feels limited, consider joining a support group for people going through breakups or dealing with mental health challenges.
Maintain or create structure. When emotions feel chaotic, routines provide a comforting sense of structure and stability. Try to eat regular meals, maintain a sleep schedule, and keep up with basic self-care even when you don’t feel like it. Physical activity is particularly powerful—exercise releases endorphins that improve mood and can reduce symptoms of depression. Even a short walk can help you feel better.
Set boundaries with your ex. For many people, limiting or cutting off contact aids the healing process—at least initially. Setting boundaries with an ex, such as limiting or cutting off contact, can aid in the healing process. This might mean unfollowing them on social media, not texting, and asking mutual friends not to share updates about your former partner. These boundaries protect your emotional space while you heal and help you focus on your own recovery.
Express your feelings. Whether through journaling, talking with trusted friends, or working with a therapist, putting feelings into words helps you process complex emotions. Journaling can be a therapeutic outlet for processing the full range of emotions after a breakup. Writing can be especially helpful for working through conflicting feelings—like missing someone while also being angry at them, or feeling relief mixed with sadness.
Give yourself permission to grieve. Acknowledge and allow yourself to grieve the loss of the relationship to aid healing. The relationship mattered, and its ending deserves to be mourned. It’s important to give yourself permission to feel and function at a less than optimal level for a while. Grief can be a natural reaction to loss, and experiencing multiple losses during a breakup is common.
Engage in activities that bring meaning. New hobbies, volunteering, or reconnecting with interests you may have neglected during the relationship can provide positive distractions and help rebuild your sense of self outside the partnership. Engaging in new hobbies or activities can help provide a positive distraction. Finding ways to stay occupied can prevent brooding and ruminating, which often worsen depression.
Consider new friendships. While you heal from the romantic relationship, building new friendships can expand your support network and remind you that meaningful connections extend beyond romantic partners. Engaging in regular self-care activities is essential to rejuvenate and heal from a breakup.
Coping Strategies to Avoid
Don’t use alcohol or drugs to numb the pain. Substances might provide temporary relief but ultimately worsen depression and delay healing. Avoiding alcohol and drugs as coping mechanisms can prevent further emotional harm after a breakup.
Avoid self-punishment or harsh self-criticism. Research shows that self-punishment is one of the maladaptive coping strategies that increases post-breakup distress. Blaming yourself entirely for the breakup or attacking your self-worth keeps you stuck in negative feelings and interferes with the healing process.
Don’t rush into new relationships. While it’s tempting to fill the void quickly, jumping into the next relationship before you’ve healed often leads to repeated patterns and additional heartache. Taking time before making major decisions after a breakup can lead to clearer judgment.
Resist the urge to isolate completely. While some alone time is healthy and necessary, withdrawing from all social contact can deepen depression, sadness, and loneliness.
How to Survive a Breakup When You’re Still in Love
Healing when you still have feelings for your ex-partner is especially painful—but it’s possible. The first step is acknowledging conflicting feelings during the grieving process, which is a natural part of recovery post-breakup. You might simultaneously miss them and know the relationship wasn’t right. Both emotions can be true.
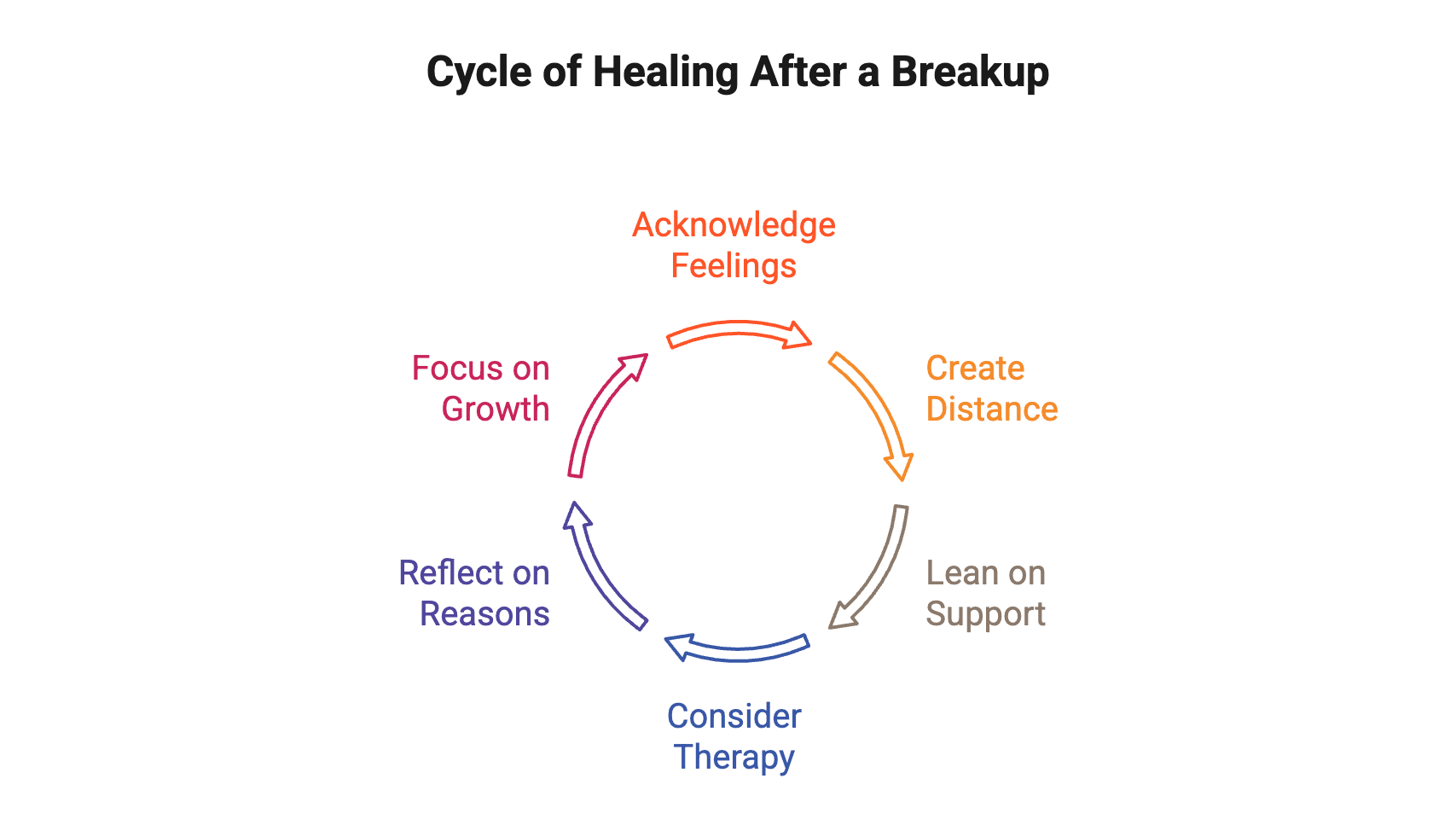
Focus on creating distance, even if it feels impossible. This means limiting contact and removing reminders from your immediate environment. Lean heavily on your support system during this time—talk about how you feel as often as you need to. Talk therapy can be especially helpful when you’re dealing with this kind of emotional complexity, as a therapist can help you process these conflicting emotions in a safe space.
Remember that love alone doesn’t make a relationship work. Many other aspects must align for a healthy partnership—compatibility, shared values, mutual respect, similar life goals. Remind yourself why the relationship ended and focus on your own growth and future relationships.
When Should You Seek Professional Help?
If your symptoms persist for more than two weeks and interfere with daily life, it’s time to talk to a mental health professional. You don’t need to suffer alone, and seeking professional help is a sign of strength, not weakness.
Consider reaching out to a clinical psychologist, therapist, or counselor if you notice:
- Depressive symptoms lasting beyond two weeks without improvement
- Inability to function at work, school, or in other relationships
- Suicidal thoughts or suicidal ideation of any kind
- Self-harm urges or behaviors
- Complete loss of interest in things that normally bring you joy
- Severe anxiety that makes it hard to leave your home
- Persistent negative feelings that don’t improve with time and self-care
If you’re in immediate danger or having thoughts of harming yourself, call 988 (the Suicide & Crisis Lifeline) or go to your nearest emergency room. Crisis support is available 24/7 and can provide immediate help when you’re in crisis.
If your low mood persists for more than a couple of weeks and affects your daily activities, reach out to a doctor or mental health professional. You should speak with a doctor if your symptoms persist or worsen after two weeks.
What Does Treatment for Depression After a Breakup Look Like?
Talk therapy is often the first-line treatment for depression following a breakup, and it can be highly effective. Cognitive behavioral therapy and other evidence-based approaches help you identify negative thought patterns, develop healthier coping strategies, and process the loss in a supportive environment. Talk therapy combined with medication is often considered when depression is severe.
A therapist with expertise in family psychology and relationship issues can help you:
- Understand how your attachment style may be affecting your recovery and future relationships
- Develop self compassion and rebuild self esteem damaged by the breakup
- Create healthy boundaries and relationship patterns for the future
- Process grief and conflicting emotions about your former partner
- Address any underlying mental health concerns that may have surfaced after the relationship ended
- Build confidence to eventually pursue new relationships when you’re ready
For some people, medication may be recommended, especially if depression is severe or doesn’t improve with therapy alone. This decision is made collaboratively with a psychiatrist or primary care doctor who can assess whether an antidepressant might be helpful. Your doctor might want you to try one or both of therapy and medication. The doctor may prescribe an antidepressant to help you cope with your emotions. It’s important to note any side effects of medications and mention them to your doctor.
A support group can also provide valuable perspectives and validation. Connecting with others who understand what you’re going through offers new coping strategies and reminds you that you’re not alone—whether through a formal group facilitated by a mental health professional or a peer support community. Support groups for those going through breakups or experiencing mental health issues can offer validation and new perspectives.
Lifestyle changes can also help cope with depression, such as exercising regularly, eating well, and maintaining healthy habits. It’s important to surround yourself with positive people who encourage you during this challenging time.
From a clinical perspective, we’ve learned that the most successful recoveries happen when clients address both the immediate pain of the breakup and the deeper patterns it reveals. We work with people to understand their attachment style, identify relationship patterns they want to change, and build skills for healthier connections in the future. Depression after a breakup is painful, but it doesn’t last forever. With time, support, and appropriate treatment, most people not only recover but develop stronger self-awareness and healthier relationship skills for the future.
Get Support in Washington, DC
If you’re struggling with your mental health after a romantic breakup in the Washington, DC area, the therapists at Therapy Group of DC in Dupont Circle are here to help. We specialize in supporting people through difficult life transitions and major life changes, including relationship loss and depression. Schedule an appointment to begin your path toward healing.
Disclaimer: This article is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or qualified mental health provider with any questions you may have regarding a medical or mental health condition. If you are in crisis or experiencing thoughts of self-harm, please call 988 (Suicide and Crisis Lifeline) or go to your nearest emergency room.