Sleeplessness Depression: Why You Wake Up at 3 AM and What It Means
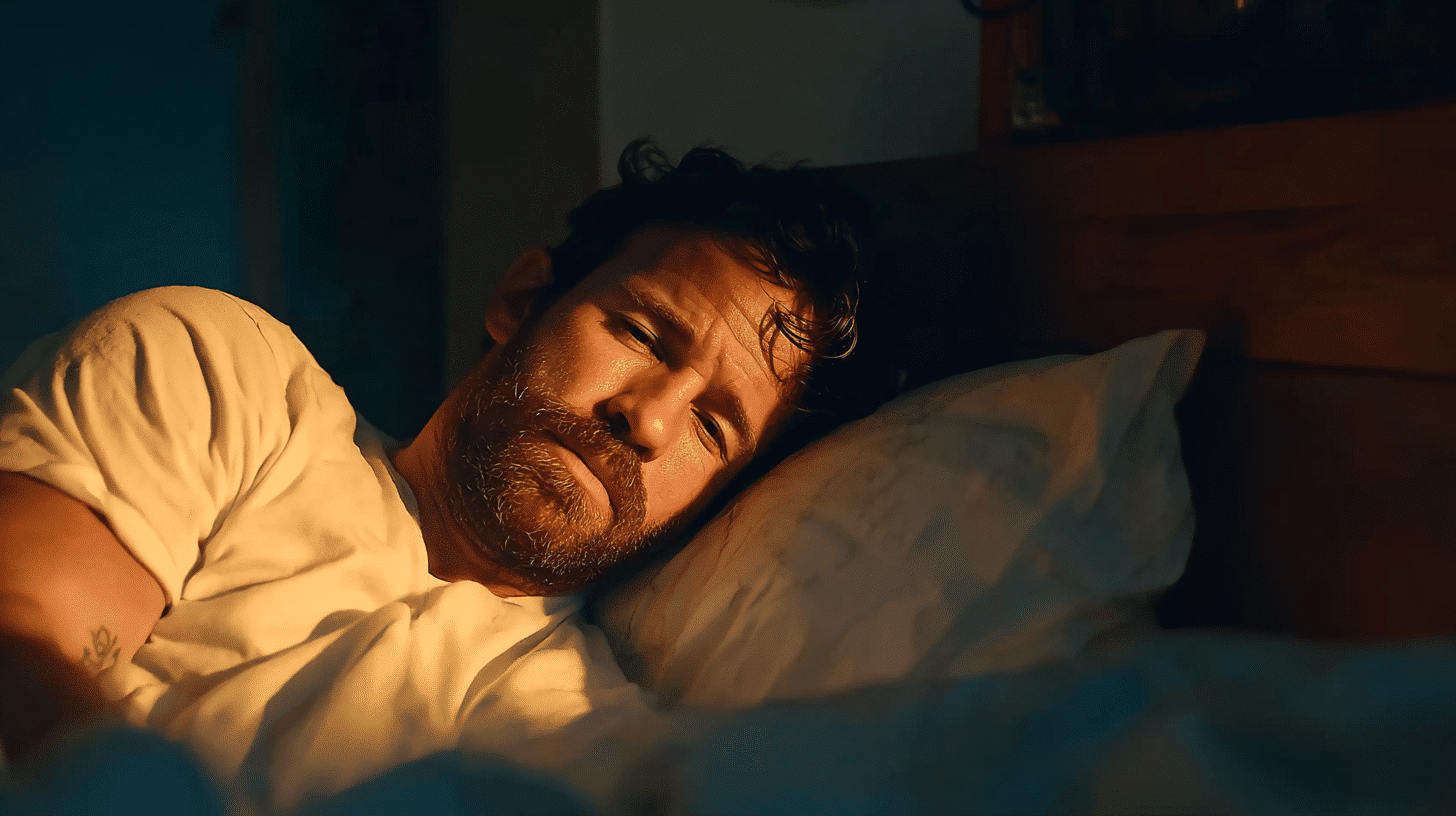
You jolt awake at 3 AM, heart racing slightly, mind already churning. The clock glows in the dark, and you know what comes next—hours of staring at the ceiling, thoughts spiraling, unable to fall back asleep. If this sounds familiar, you’re experiencing one of the most common yet distressing symptoms of depression: middle-of-the-night awakening.
Sleeplessness and depression are deeply connected, affecting most people with depression. While many people associate insomnia with trouble falling asleep, waking up in the early morning hours and being unable to return to sleep is equally common—and equally exhausting. Sleep is critical to both physical and mental health, and understanding why this happens can help you find better solutions.
Why Does Depression Cause Middle-of-the-Night Waking?
Depression disrupts your body’s stress response system, specifically the hypothalamic-pituitary-adrenal (HPA) axis—the system that controls cortisol production. When this system malfunctions, it leads to abnormal cortisol levels that interfere with your natural sleep patterns.
Cortisol is often called the “stress hormone,” and it normally follows a predictable pattern—low at night when you sleep, rising in the early morning to help you wake up. But depression elevates cortisol at the wrong times, leading to a state of hyperarousal that makes sleep difficult. Your body gets stuck in an alert state when it should be resting.
This is why you might fall asleep initially but then wake up a few hours later unable to get back to sleep. Your brain has shifted into a hyper-vigilant state that’s incompatible with deep, restorative sleep. Sleep deprivation then increases negative emotional responses to everyday stressors, creating a cycle where poor sleep intensifies depression symptoms.
What Role Does Rumination Play in 3 AM Waking?
Rumination—repetitive negative thinking—keeps your mind active at night, making it nearly impossible to fall back asleep once you wake up. When you’re depressed, your brain gets stuck in loops of worry, regret, or problem-solving that intensify in the quiet darkness.
These racing thoughts aren’t just annoying—they’re a core feature of how depression affects sleep. Your mind may replay conversations, worry about tomorrow, or fixate on problems that feel unsolvable. The lack of daytime distractions makes these thoughts feel louder and more urgent at 3 AM than they did at 10 PM.
In our work with clients experiencing middle-of-the-night waking, we’ve noticed that simply telling someone to “stop thinking” or “clear your mind” rarely works—and often makes them feel worse about their inability to sleep. The rumination isn’t a willpower problem; it’s driven by the same neurobiological changes that cause depression itself. We help clients develop specific techniques for when rumination hits, like keeping a “worry journal” by the bed or using progressive muscle relaxation to redirect attention away from racing thoughts.
How Does Depression Fragment Your Sleep?
Beyond waking at specific times, depression causes fragmented sleep—multiple awakenings throughout the night and difficulty transitioning between sleep stages. Stress hormones and disrupted circadian rhythms work together to create a pattern of shallow, restless sleep.
People with insomnia are 10 times more likely to develop depression than those who sleep well. But the relationship works both ways: poor sleep can increase the risk of developing depression in the first place, and ongoing poor sleep worsens existing depression symptoms. Lack of quality sleep intensifies depression, creating a cycle where each condition reinforces the other.
You might notice that even when you do sleep, you wake up feeling unrefreshed. That’s because depression prevents you from reaching the deeper stages where physical and mental restoration happen.
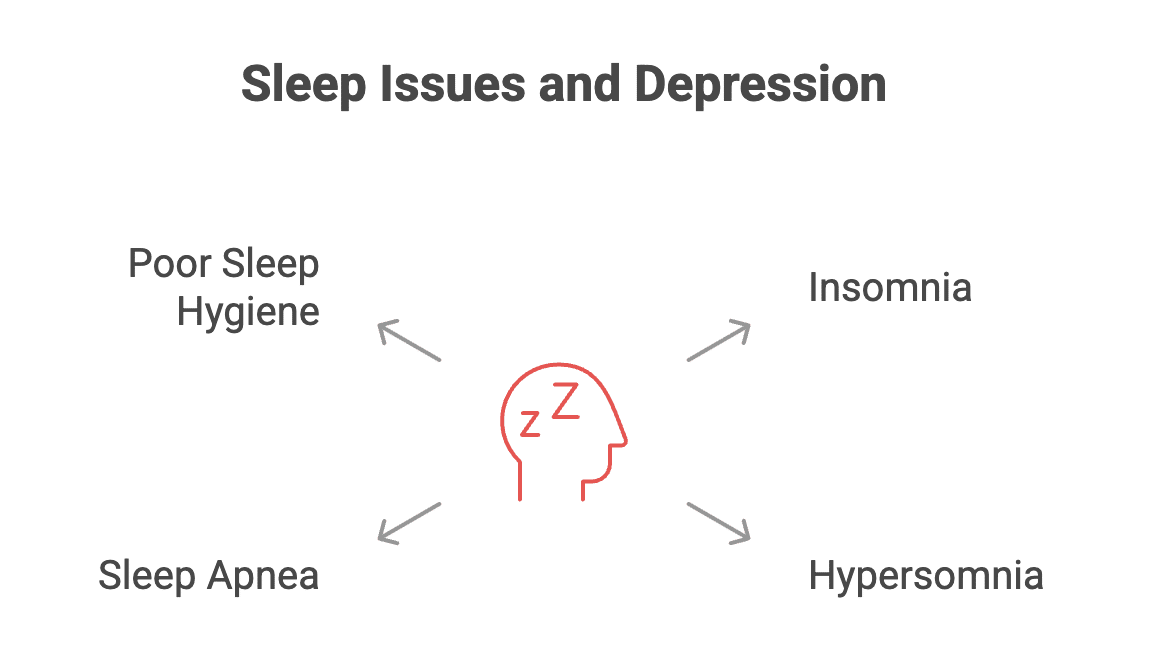
What Other Sleep Issues Happen with Depression?
While middle-of-the-night waking is common, depression affects sleep in several ways:
- Insomnia (difficulty falling asleep or staying asleep)
- Hypersomnia (sleeping too much but still feeling exhausted)
- Sleep apnea (breathing disruptions that worsen both sleep and mood)
Many people with insomnia also have clinical depression, and most patients with clinical depression experience bouts of insomnia. These aren’t separate problems—they’re interconnected symptoms that need to be addressed together. Conditions like sleep apnea or restless legs syndrome can co-occur with depression and contribute to sleeplessness.
Does Poor Sleep Hygiene Make It Worse?
Poor sleep habits intensify problems when you’re already dealing with depression. An inconsistent sleep schedule, screen use before bed, large meals in the evening, or caffeine and alcohol consumption can all worsen sleeplessness. Avoiding alcohol is particularly important—it may help you fall asleep initially but disrupts sleep quality and can worsen depressive symptoms.
However, it’s important to recognize that depression-related sleep problems go beyond simple habit changes. You can follow perfect sleep hygiene and still wake up at 3 AM because of the underlying biological and psychological factors at work. Practicing good sleep hygiene is crucial, but it’s often not sufficient on its own.
Can Treating Sleep Problems Help Depression?
Yes—and this is one of the most hopeful findings in recent research. Treating insomnia directly improves both sleep and mood, even when depression is still present. You don’t have to wait until your depression is “cured” to address your sleep problems. In fact, identifying and addressing sleep problems early is important for alleviating the severity of psychiatric disorders, including depression.
Cognitive Behavioral Therapy for Insomnia (CBT-I) is the first-choice treatment for chronic insomnia and works by changing the thoughts and behaviors that keep you from sleeping. This therapeutic model helps individuals cope with depression and sleep-related thoughts simultaneously. Studies show it’s more effective long-term than sleep medications and has fewer side effects.
Digital CBT-I programs make this treatment more accessible through apps and online platforms, and research confirms they help improve both sleep quality and depressive symptoms. The treatment addresses rumination, sleep anxiety, and counterproductive habits at the same time.
We often recommend CBT-I alongside traditional talk therapy for depression, and we’ve consistently seen how addressing sleep directly accelerates overall improvement. One pattern we notice is that clients feel more equipped to work on their depression when they’re getting better sleep—their capacity for emotion regulation, problem-solving, and engaging in therapy increases significantly. Treating both conditions together isn’t just more effective; it gives people a sense of progress early in treatment when they need it most.
What About Medications?
Sometimes sleep medications or antidepressants are part of treatment, but they’re not the first choice for sleep problems. Therapy-based approaches like CBT-I work better in the long run and don’t carry the same risks of dependency or side effects.
That said, certain medications—including some antidepressants—can cause insomnia or daytime drowsiness that disrupts your sleep cycle further. If you’re taking medication and experiencing new or worsening sleep problems, talk to your doctor about adjusting your treatment.
What Can You Do Right Now?
If you’re waking up at 3 AM and struggling with depression, here are evidence-based steps that can help:
- Talk to your doctor about both sleep and mood symptoms—they need to be addressed together
- Keep a regular sleep schedule, even on weekends, to stabilize your circadian rhythm
- Get up if you can’t sleep after 20 minutes—staying in bed awake worsens sleep anxiety
- Avoid checking the clock—knowing the exact time increases stress and rumination
- Limit caffeine after noon and avoid alcohol in the evening
- Get bright light exposure early in the day to regulate your sleep-wake cycle and improve mood
- Exercise regularly—physical activity can significantly decrease symptoms of depression and improve sleep quality
- Keep naps brief (10-20 minutes) if needed, as short naps can help regulate emotions without disrupting nighttime sleep
Ready to Get Support?
If you’re in the Dupont Circle area and looking for support with sleeplessness and depression, the therapists at Therapy Group of DC are here to help. We understand how exhausting it is to face each day without adequate rest, and we can work with you on evidence-based approaches that address both sleep and mood. Consulting a healthcare provider is essential for proper diagnosis and treatment of sleep and mood disorders. Schedule an appointment to get started.
Frequently Asked Questions About Sleeplessness and Depression
What are common sleep disorders associated with depression?
Depression is often linked with several sleep disorders, including insomnia disorder, hypersomnia, and obstructive sleep apnea. These common sleep disturbances can cause excessive daytime sleepiness, prolonged sleep latency, and fragmented sleep, further complicating depressive symptoms.
How do sleep and circadian rhythms affect depression?
Disruptions in the body’s internal clock and sleep regulation, including altered REM sleep patterns and circadian rhythms, can worsen major depressive disorder. These disturbances impact sleep quality and mood, making it essential to maintain a consistent sleep schedule to promote sleep health.
Can improving sleep help treat depression?
Yes, addressing sleep difficulties through cognitive behavioral therapy, sleep restriction techniques, and good sleep hygiene can significantly improve both sleep quality and depressive symptoms. Consulting a sleep specialist or mental health provider can help tailor treatments for better outcomes.
What role does rapid eye movement (REM) sleep play in depression?
Rapid eye movement sleep is crucial for emotional regulation and memory consolidation. Depressed patients often experience altered REM sleep, such as shortened latency or increased density, which may serve as biomarkers for primary depressive disease and influence treatment strategies.
When should someone seek help from a sleep specialist?
If sleep problems persist despite practicing good sleep habits or if there are symptoms like excessive daytime sleepiness, difficulty with sleep onset, or signs of sleep apnea, it is important to consult a sleep specialist. Early intervention can prevent worsening of mental health disorders and improve overall sleep medicine outcomes.
Disclaimer: This article is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or qualified mental health provider with any questions you may have regarding a medical or mental health condition. If you are in crisis or experiencing thoughts of self-harm, please call 988 (Suicide and Crisis Lifeline) or go to your nearest emergency room.