Depression Versus Sadness: Why Depression Isn’t “Just Feeling Sad”
“You’re just sad—snap out of it.” If you’re experiencing depression, you’ve probably heard this. It’s one of the most harmful misconceptions about mental health. Depression and sadness share surface similarities, but they’re fundamentally different experiences. Sadness is a common emotion everyone feels, while depression is a medical condition that affects your brain, body, and daily life in ways that go far beyond feeling down.
Understanding these differences helps you recognize when you or someone you care about might need professional support—and challenges the stigma keeping people from seeking mental health care.
What Are the Two Main Differences Between Sadness and Depression?
Duration and impact on functioning separate sadness from depression. Sadness is a temporary emotion that fades within days or weeks. Depression persists for at least two weeks and often much longer. More critically, sadness doesn’t stop you from living your life, but depression interferes with work, personal relationships, and everyday tasks.
When you feel sad after disappointing events or upsetting life events, you can usually still function. You might feel down about losing a job or ending a relationship, but you can still get out of bed, eat meals, and connect with loved ones. Sadness exists on a continuum with normal well-being—it’s part of the natural range of human emotions.
Depression operates differently. Depression is a mood disorder classified in the Diagnostic and Statistical Manual that involves persistent changes in how your brain processes emotions, energy, and motivation. Depression requires at least five symptoms present for two weeks, including either depressed mood or loss of interest. These symptoms of depression must cause significant distress or impairment in daily life. People of any age, gender, and race can develop this ongoing mental health disorder.
In our practice, we often hear people say “I’ve been sad before, so I know what depression is.” But the clients we work with who’ve experienced both describe depression as fundamentally different. Sadness has texture—you can feel its edges, understand its source. Depression feels like numbness, like moving through fog. One client described it as “sadness is crying at a sad movie; depression is not being able to feel anything while watching a sad movie.” That distinction helps families understand why encouragement alone doesn’t work.
Why Do I Feel Deep Sadness?
Feeling sad is a normal reaction to loss, rejection, disappointment, or stress. Your brain responds emotionally to negative events—this is healthy and adaptive. Sadness helps you process difficult experiences, signals that you need support, and motivates change when something isn’t working.
Common specific triggers for a sad mood include:
- Relationship problems or breakups
- Loss of a family member or friend
- Work stress or job loss
- Financial difficulties
- Major life transitions
- Health challenges
The key: sadness has identifiable causes and improves as you process the event. You might feel sad for days after an argument, but as you talk things through, the feelings fade. This is why sadness is a common temporary emotion rather than an ongoing mental health disorder.
Depression may have no identifiable cause. You might feel deeply depressed even when circumstances seem manageable. Depression involves biological and psychological changes beyond simple life stress—brain chemistry imbalances, genetics, hormonal changes, and risk factors can trigger depression independent of external events.
What Makes Depression a Medical Condition?
Depression is a medical diagnosis involving measurable brain changes, physical symptoms, and clear diagnostic criteria. Unlike sadness, major depressive disorder and other mental disorders require clinical evaluation by a mental health professional.
Symptoms extend far beyond how a person feels emotionally. Common symptoms of depression include:
- Physical symptoms: Changes in appetite, weight gain or loss, trouble sleeping or sleeping too much, muscle pain, body aches, persistent fatigue that doesn’t improve with enough sleep
- Cognitive changes: Difficulty concentrating, memory problems, slowed thinking, trouble making decisions
- Behavioral shifts: Lose interest in activities you once enjoyed, withdraw socially, struggle to complete routine tasks
- Severe psychological symptoms: Low self esteem, feelings of worthlessness or guilt, suicidal thoughts or suicidal ideation, and in extreme cases, suicide attempts
People experiencing depression cannot “snap out of it” through willpower alone. Brain changes in major depression affect neurotransmitter systems regulating mood, energy, and pleasure. This is why depression typically requires professional treatment—talk therapy, antidepressant medication, or both approaches combined.
How Does Depression Affect Daily Life Differently Than Sadness?
Depression impairs everyday functioning in ways sadness doesn’t. When you feel sad, you might skip a social event or need extra support, but you can generally handle responsibilities. Depression creates barriers that make basic tasks feel impossible, no matter how much a person feels motivated to try.
People experiencing depression often describe:
- Inability to get out of bed or complete morning routines
- Missing work or school repeatedly due to severe symptoms
- Neglecting self-care like showering, eating regular meals, or taking prescribed medication
- Complete withdrawal from friends and family members in the same household
- Inability to feel pleasure during previously enjoyable activities
- Disproportionate amount of time spent in bed or isolated
This level of impairment distinguishes clinical depression from a passing sad mood. A healthcare professional evaluates not just emotions, but how depression affects relationships, work performance, daily responsibilities, and your capacity for positive emotions.
One of the most revealing questions: “Can you function?” Someone who’s sad can usually push through to get to work, care for their kids, or show up for obligations even if they don’t feel like it. Someone with depression often physically cannot, no matter how much they want to. We’ve seen high-achieving clients who never missed a day of work suddenly unable to answer emails or get dressed. That functional collapse is the clearest signal.
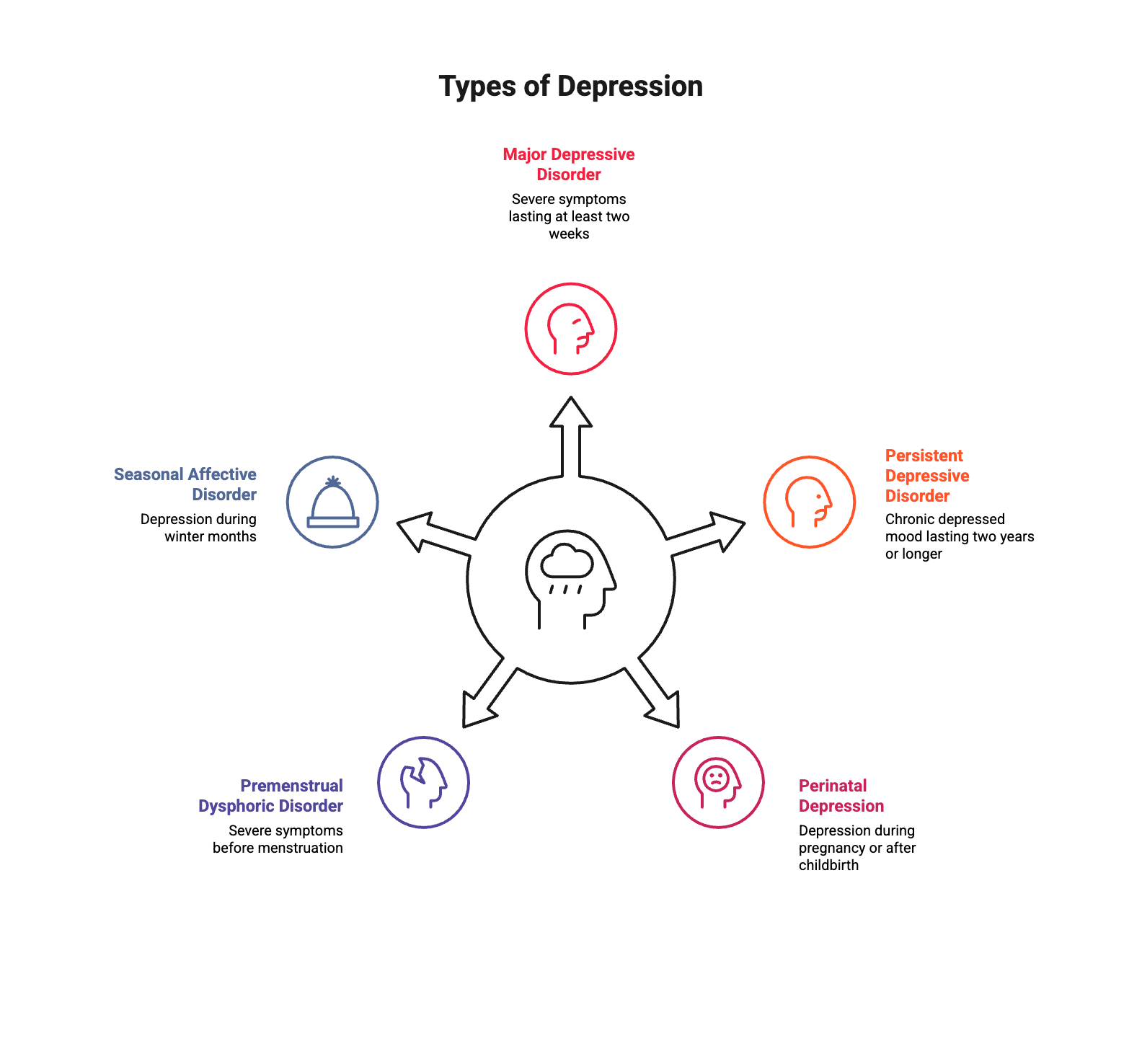
What Are the Different Types of Depression?
Understanding sadness and depression requires recognizing that depression encompasses several mood disorders. Each type shares core features but has unique characteristics affecting treatment approaches and mental health outcomes.
Major depressive disorder is most common, with severe symptoms lasting at least two weeks that significantly impair functioning. The condition affects millions and responds well to evidence-based treatment approaches.
Persistent depressive disorder involves chronic depressed mood lasting two years or longer. While symptoms may be less intense than major depression, the persistent nature creates substantial challenges for mental health and quality of life.
Perinatal depression affects people during pregnancy or after childbirth. This isn’t “baby blues”—perinatal depression involves the same symptoms of depression as major depression but occurs around pregnancy. Hormonal changes, sleep deprivation, and life adjustments all contribute as risk factors. Perinatal depression requires specialized mental health support because it affects both parent and child.
Premenstrual dysphoric disorder (PMDD) causes severe symptoms the week before menstruation, including mood swings, irritability, breast tenderness, and extreme sadness that improve once menstruation begins. PMDD differs from premenstrual syndrome (PMS) due to symptom severity and impact on functioning.
Seasonal affective disorder follows a seasonal pattern, typically during winter when daylight hours are shorter. Other symptoms mirror major depression but follow a predictable annual cycle.
How Do You Know When to Seek Help?
If low mood persists beyond two weeks and affects functioning, consult a healthcare professional for a medical diagnosis. The two-week threshold distinguishes temporary sadness from potential depression, though you should seek support immediately if symptoms are severe or create immediate danger.
Call the local emergency services number (911) or crisis line right away if you or someone experiences:
- Suicidal thoughts or plans for self harm
- Thoughts of hurting others
- Immediate danger due to severe symptoms
- Inability to care for basic needs
For non-emergency support, contact a mental health professional, your primary care physician, or call the National Suicide Prevention Lifeline at 988. Early intervention improves outcomes and reduces suffering.
What Treatment Options Exist for Depression?
Depression treatment typically involves talk therapy, antidepressant medication, or both. Unlike sadness, which resolves on its own, depression usually requires professional intervention to improve. Treatment helps restore functioning and reduces the risk of future episodes.
Effective talk therapy approaches include:
- Cognitive behavioral therapy (CBT): One of the most common and effective forms of psychotherapy, CBT identifies and changes negative thought patterns maintaining depression
- Interpersonal therapy: Addresses relationship issues and life transitions contributing to depression
- Psychodynamic therapy: Explores how past experiences affect current mood and self esteem
Antidepressant medication adjusts brain chemistry imbalances involved in depression. Your healthcare professional’s medical opinion determines whether medication alone or combined with therapy is recommended. Antidepressants may produce some improvement within the first week, but full benefits typically take several weeks to months. Recovery may require trying several medications to find what works best, and patients usually continue antidepressants for at least six months after symptoms improve to prevent relapse.
Simple lifestyle changes support recovery, though they’re not substitutes for professional treatment. Regular exercise, quality sleep, healthy eating, limiting alcohol, and maintaining connections with loved ones all help reduce symptoms. Addressing vitamin deficiencies and incorporating self help strategies like mindfulness can also improve mental health.
For severe depressive episodes not responding to standard treatment, additional options include Electroconvulsive Therapy (ECT), transcranial magnetic stimulation, or specialized medication regimens.
How to Pull Yourself Out of a Depressive Episode?
Professional treatment is the foundation for recovering from depression, but self help strategies support the process. While you can’t simply “pull yourself out” through willpower, certain actions help manage symptoms and support recovery alongside professional care.
Strategies that support mental health during depression:
- Maintain a routine even when you don’t feel motivated
- Set small, achievable goals rather than overwhelming yourself
- Stay connected with trusted friends or support groups—peer support helps many people find support
- Practice mindfulness to stay present rather than ruminating
- Move your body regularly, even brief walks help
- Seek support early rather than waiting for symptoms to worsen
These self help approaches work best when combined with talk therapy or antidepressant medication prescribed by a healthcare professional. Depression is a medical condition requiring treatment—simple lifestyle adjustments alone rarely resolve clinical depression, though they enhance formal treatment outcomes.
Can You Have Both Sadness and Depression?
Yes—sadness can be both a symptom of depression and a separate emotional response. Someone with depression might feel sad about a specific loss while experiencing the broader constellation of symptoms. The difference lies in whether sadness is the only experience or part of a larger pattern affecting mental health and functioning.
Key takeaways about sadness and depression:
- Sadness is a common emotion and temporary emotion; depression is an ongoing mental health disorder
- Sadness has specific triggers; depression may have no identifiable cause
- You can function through sadness; depression interferes with daily life
- Sadness resolves without treatment; depression requires professional mental health support
- Sadness lasts days or weeks; depression persists for months or years without intervention
The presence of other symptoms—like loss of pleasure, difficulty concentrating, physical symptoms, changes in sleep or appetite, low self esteem, and extreme sadness disproportionate to circumstances—signals depression rather than simple sadness.
What Role Does Stigma Play?
The misconception that depression is “just sadness” perpetuates harmful stigma preventing people from getting mental health care. When depression gets minimized to a character flaw, people feel ashamed about symptoms they can’t control. This shame keeps them isolated, unable to seek support from caring counselors or tell loved ones what they’re experiencing.
Language matters when discussing mental health. Phrases like “snap out of it,” “just think positive,” or “everyone gets sad sometimes” invalidate depression’s serious nature as a medical condition. These comments suggest weakness rather than a legitimate mood disorder requiring treatment.
Challenging stigma requires education about how mental disorders actually work. Depression isn’t a choice, moral failing, or weakness. It’s a treatable medical condition affecting millions across all demographics. Seeking help from a mental health professional demonstrates strength and self-awareness, not weakness. The more we normalize mental health care, the more people can find support without shame.
How Can You Support Someone With Depression?
Supporting someone experiencing depression means recognizing it’s not sadness you can fix with advice. Your loved ones with depression need patience, compassion, and encouragement to access therapy and professional mental health support.
Helpful ways to support include:
- Listen without judgment or trying to fix everything immediately
- Validate their experience without minimizing it to normal sadness
- Help them find support through a licensed therapist or online service
- Offer practical help with overwhelming tasks like groceries, childcare, or appointments
- Learn about depression, risk factors, and treatment so you understand their experience
- Check in regularly, even if they don’t respond
Avoid toxic positivity or suggesting they overcome depression through attitude alone. Comments like “just think happy thoughts” don’t help and increase isolation. Depression requires proper treatment from caring counselors and mental health professionals, not platitudes.
If you’re concerned about suicidal thoughts or plans for self harm, ask directly. Asking doesn’t plant ideas—it opens doors for honest conversation and potentially life-saving intervention. If they express intentions around suicide attempts or immediate danger, help them contact a volunteer crisis counselor, mental health professional, or the local emergency services number immediately. Never leave someone alone if you believe they’re at risk.
Get Support for Depression in Washington, DC
If you’re struggling to understand whether what you’re experiencing is sadness or something more, the therapists at the Therapy Group of DC can help. We provide compassionate, evidence-based mental health care for depression and related concerns in our Dupont Circle office. Schedule an appointment to start feeling better.
Disclaimer: This article is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or qualified mental health provider with any questions you may have regarding a medical or mental health condition. If you are in crisis or experiencing thoughts of self-harm, please call 988 (Suicide and Crisis Lifeline) or go to your nearest emergency room.