How To Help Partner With Depression
Depression is common and treatable. It is an illness, just like any other medical condition, and deserves understanding and proper care. Depression is a diagnosable mental health condition with complex causes relating to genetics, biology, and environmental factors.
This article will provide guidance on how to support a depressed partner with empathy and practical strategies. When it shows up in a relationship, support works best when it’s caring, concrete, and paced for low energy days. If there’s immediate danger, contact emergency services right away or call/text 988.
What are the common signs of depression in a partner?
Depression is more than a bad day. Watch for a cluster of symptoms that show up most days for two or more weeks and get in the way of daily life. Changes in behavior, such as withdrawal or increased irritability, are key aspects of recognizing depression in a partner. A depressed person is not just feeling blue or having a bad day; their condition involves brain chemistry changes. A clear, plain‑language overview is in the National Institute of Mental Health’s guide to depression.
- Low mood or irritability
- Losing interest in things that used to be enjoyable
- Sleep or appetite changes
- Low energy and trouble concentrating
- Pulling away from friends and family, or feeling hopeless or guilty
- Increased anger or irritability
- Red flags: talk about death or self‑harm, giving away important items, or a sudden calm after severe distress (treat as urgent)
Recognizing depression often involves observing changes in behaviors and behavior patterns, including anger, withdrawal, and other emotional symptoms. Depression can show up in unexpected ways, and common depression symptoms are often easy to miss. Early awareness of these signs is crucial for providing support.
How is depression different from a “rough patch” or burnout?
A rough patch lifts with rest or a good weekend. Depression sticks, flattens enjoyment, and touches most parts of life. Unlike a rough patch, depression can be influenced by personality traits and life experiences, which contribute to its development and persistence. Clinicians look for duration (≥2 weeks), severity (it disrupts school, work, or home), and breadth (it shows up across settings). Effective treatments exist—therapy, medication, or both—as summarized in a recent JAMA review of adult depression care.
How do I bring it up without making things worse?
Choose a low‑stress moment, lead with care and curiosity, and stick to what you’ve noticed—not judgments or quick fixes. Instead of offering advice, ask your partner specific questions about what they need or how you can support them. Listening is essential—give your partner your full attention and encourage them to speak openly about how they feel.
- Private, unrushed, and distraction‑light
- Use specific, kind observations: “I’ve noticed you’re sleeping a lot and skipping things you usually enjoy.”
- Express that you are concerned in a gentle, non-judgmental way: “I’m concerned about you, and I care. You can talk to me about anything.”
- Validate first, problem‑solve later: “You don’t have to explain everything right now. I’m here.”
- Ask permission for next steps: “Would a short walk help, or should we sit quietly?”
What words can I use?
- “I care about you and I’m not going anywhere.”
- “Your emotions are valid, and I’m here to support you.”
- “I’m not here to fix it. I want to understand.”
- “I know things are hard, but I have hope we can get through this together.”
- “Can we pick one small thing to try today—like a light meal or a short walk?”
What should I avoid saying?
- Minimizing: “Everyone gets sad.”
- Cheerleading over feelings: “Just think positive.”
- Comparisons: “When I was low, I just…”
- Moral judgments: “You should…,” “Why can’t you just…?”
- Jumping to offering solutions: “Have you tried just…?”
How can we make daily life easier together?
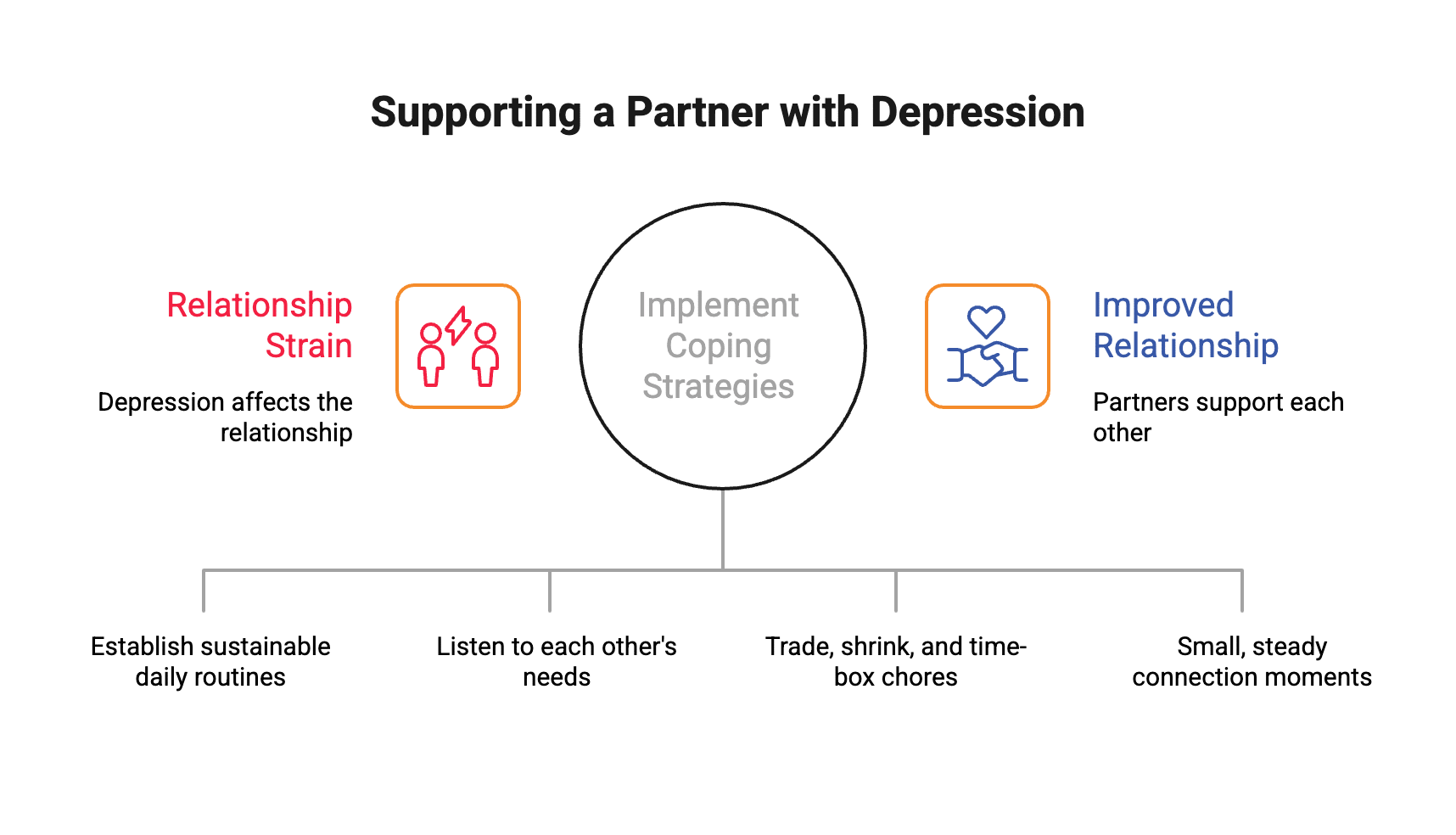
Lower the bar on non‑essentials and add gentle structure you both can sustain. Coping strategies, such as micro‑routines (consistent wake time, a little fresh air, simple meal anchors), can help both partners manage daily challenges and support each other when partner struggles with depression affect your relationships. Work with your partner to break down overwhelming tasks into smaller, manageable steps to build motivation.
Try a 10‑minute daily check‑in and low‑pressure time together. Maintaining a healthy routine supports your well-being and helps you both cope with emotional and practical challenges. Small shifts—like morning light by a window and a “good‑enough” tidy zone—reduce friction.
Tips for coping with daily life when supporting a partner with depression:
- Communicate openly and listen to each other’s needs.
- Encourage healthy habits like regular meals and sleep.
- Set realistic expectations and celebrate small wins.
- Take time for self-care to support your own well-being.
How do we share tasks when energy is low?
Make the week lighter on purpose—trade, shrink, and time‑box chores so they’re doable on low‑energy days. Even small changes can make a big difference for a significant other when energy is low.
- Pick a few “must do” items (meds, mail, meals) and let the rest be “nice to do.”
- Create a simple, kind shared list on the fridge.
- Use short work blocks (10–20 minutes) and a visible stop time.
- Celebrate progress, not perfection.
How do we stay close when intimacy dips?
Connection can be small and steady—think micro‑moments, not grand gestures.
When intimacy dips, it’s common to face emotional challenges, both for you and your partner. Supporting a partner who is struggling with these emotions means offering understanding, patience, and empathy as they navigate difficult feelings.
- Try daily check‑ins, a brief walk, shoulder‑to‑shoulder time (cooking, folding), and non‑sexual touch.
- Name what feels good right now and what’s off‑limits for the moment.
- Curiosity beats criticism; appreciation beats advice.
How do I encourage professional help?
Normalize care, offer hands‑on help with logistics, and suggest a short trial (for example, three sessions) to lower the bar. Seeking professional support is crucial—encourage your loved one to seek help from a mental health professional or doctor for a depression diagnosis and treatment. Gently and consistently remind your partner that asking for help is not a sign of weakness. Finding support can include reaching out to support groups, online therapy platforms, or local resources.
- Options: primary‑care visit, therapy, and/or medication. For what therapy looks like, see NIMH’s overview of psychotherapies. For medicines and common questions, see NIMH’s page on mental health medications.
- Logistics you can share: search together, send a first message, offer a ride or to wait in the lobby, help track questions and wins between sessions.
- Finding care: if you need a broader search, the SAMHSA treatment locator lists mental‑health services by ZIP code.
What if my partner refuses help for now?
Stay supportive and keep the door open. It’s normal to feel frustrated or worried when your partner refuses help, but remember that your concern is valid. Focus on small daily steps while you set humane limits for yourself. You can also consult a therapist yourself to learn how to respond, set boundaries, and watch for red‑flag changes. Revisit the idea of care at calmer times; readiness shifts.
When is it an emergency?
Any talk of suicide or self‑harm, escalating substance use with safety risks, or inability to care for basic needs is urgent. In these situations, it is important to recognize the risk of suicide and remove access to alcohol and drugs to help ensure safety. In those moments, contact emergency services or the 988 Suicide & Crisis Lifeline.
How do I care for myself while supporting them?
Your steadiness helps both of you. As a family member or loved one supporting someone with depression, it is essential to practice self care and engage in self care activities to maintain your own well-being. Maintain your own well-being by seeking support for yourself to avoid burnout. Keep your own supports active and set limits early—before resentment builds. Protect the basics (sleep, movement, meals), keep one or two personal joys on the calendar, and rotate in friends/family for practical help.
Consider joining support groups for family members and loved ones of people with depression, as these can provide emotional support, advice, and validation. For more ideas, see NIMH’s guide to caring for your mental health.
About Therapy Group of DC
Warm, evidence‑based care in Dupont Circle with therapists experienced in depression and couples concerns. When you’re ready, you can explore care at the Therapy Group of DC. Inclusive and affirming.
Frequently Asked Questions About Supporting a Partner with Depression
How can I practice active listening when my partner is feeling sad?
Active listening means giving your partner your full attention without interrupting, judging, or offering immediate solutions. Reflect their feelings back to them to show understanding and create a safe space for open communication during this difficult time.
What should I do if my partner refuses professional help?
If your partner is not ready for professional help, stay patient and supportive while keeping the door open. Encourage small daily steps toward recovery and consider seeking support for yourself to manage the emotional toll.
How important is enough sleep for someone struggling with depression?
Getting enough sleep is critical for mental health and recovery. Encouraging your partner to maintain a regular sleep schedule can improve mood and energy levels, making it easier to cope with depression.
What resources are available in a crisis?
In a critical situation, such as when your partner talks about self-harm or suicide, contact emergency services immediately. The 988 Suicide & Crisis Lifeline is a vital resource for urgent mental health support.
How can social activities help my depressed spouse?
Engaging in social activities, even in small ways, can help reduce feelings of isolation and support emotional well-being. Encourage your spouse to participate at a comfortable pace to foster connection and hope.