Is It Depression or Just Perimenopause? Understanding Mood Changes in Your 40s and 50s
If you’re in your 40s or 50s and feeling more tearful, irritable, or sad than usual, you might wonder whether these mood changes are just part of perimenopause or something more serious. Perimenopause and depression are closely connected—about 1 in 5 women experience depression during the menopause transition, making it a vulnerable time for women’s health and mental health. Research shows depression is significantly more common during perimenopause than at other life stages, and depressive symptoms can be mistaken for typical symptoms of perimenopause, which is why understanding the difference matters for getting the right support.
What are the emotional symptoms of perimenopause?
Perimenopause brings a wide range of mood symptoms that can feel confusing and overwhelming. About 4 in 10 perimenopausal women experience mood symptoms during perimenopause that are similar to PMS, including irritability, mood swings, and feeling more emotional than usual. You might notice you’re crying more easily, snapping at loved ones, or feeling anxious about things that didn’t bother you before.
These emotional states happen because hormonal fluctuations during perimenopause directly impact brain neurochemistry. During perimenopause, the ovaries begin producing less estrogen, and as estrogen levels decrease, hormonal balance with progesterone is disrupted. As estrogen levels fluctuate widely and irregularly, they affect neurotransmitters like serotonin and dopamine, which are crucial for mood regulation. Hormone levels can swing dramatically from day to day during perimenopause, and this unpredictability makes mood symptoms harder to manage than the more stable hormone patterns most women experienced during their reproductive years.
Common symptoms during perimenopause include:
- Feeling more irritable or having a shorter fuse
- Mood swings that seem to come out of nowhere
- Increased tearfulness or emotional sensitivity
- Anxiety or constant worrying
- Feelings of sadness or hopelessness
- Difficulty concentrating or brain fog
In our practice, we see many women who describe their perimenopausal mood symptoms as intensified versions of their usual emotional responses. Many describe feeling like they’re “walking around without their usual emotional buffer.” This pattern is important to recognize: perimenopause can amplify emotional responses you already have, making everyday stressors feel harder to manage. Understanding this helps normalize the experience while also recognizing when support might help.
The challenge is that these perimenopausal symptoms can occur for years without a clear pattern, unlike typical PMS that follows your menstrual cycle. Perimenopause is a period of time where women have changes in their menstrual cycle patterns. Some perimenopausal women may experience erratic or irregular menstrual cycles during perimenopause, and mood symptoms may not line up predictably with periods anymore.
When Mood Changes Signal Depression
While mood changes are common during the menopause transition, perimenopausal depression is different. Depression during perimenopause generally comes on gradually, not suddenly, and involves symptoms of depression that are more persistent and severe than typical mood swings. Women experiencing perimenopausal depression often disconnect from social activities and feel significant guilt about it.
Depression manifests as a general sense of hopelessness, losing interest in normal activities, and feeling disconnected from others. This mental health condition goes beyond regular mood changes. The key difference is duration and impact: if you’re experiencing depressive symptoms lasting more than two weeks that affect your ability to work, maintain relationships, or enjoy life, this goes beyond typical perimenopausal symptoms and warrants professional support.
How do I know if it’s menopause or depression?
The overlap between perimenopause symptoms and major depression makes diagnosis tricky, which is why depression is sometimes mistaken for normal menopause symptoms. Both clinical depression and perimenopausal depression can cause sleep problems, trouble concentrating, changes in appetite, and fatigue. However, there are important distinctions between major depressive disorder and mood disorders related to hormonal changes.
Physical symptoms like hot flashes, night sweats, and vaginal dryness are specific to the menopause transition and don’t typically occur with depression alone. Common perimenopausal symptoms like hot flashes and night sweats significantly disrupt sleep and can substantially increase the risk of developing depressive symptoms—some research suggests up to 10 times higher. These menopausal symptoms and other physical symptoms create interrupted sleep, which then creates a vicious cycle—poor sleep can hinder decision making and increase emotional instability during perimenopause.
Signs that point more toward clinical depression include:
- Persistent feelings of hopelessness or emptiness most of the day
- Losing interest in activities you used to enjoy
- Thoughts of self-harm or that life isn’t worth living
- Significant changes in appetite or weight (not related to other symptoms)
- Pervasive lack of motivation that affects daily functioning
- Sleep problems including trouble sleeping or sleeping too much beyond what hot flashes cause
These symptoms of depression differ from typical mood changes during perimenopause and require professional evaluation.
Anxiety can occur alongside depression during perimenopause, involving constant worrying and physical symptoms such as muscle tension. Women in their 40s and 50s often face additional life stressors—caring for aging parents, children leaving home, career pressures—that can affect mental health and make distinguishing between causes more complex.
We frequently see clients who’ve been told their mood symptoms are “just menopause” and to wait it out. This dismissive response can be harmful and delays needed care. If your mood changes are affecting your quality of life, relationships, or ability to function, those symptoms deserve attention regardless of whether they’re related to hormonal changes, depression, or both. Your experience is valid, and effective treatment options exist.
Certain women are at increased risk for perimenopausal depression, including those with a prior history of depression, anxiety disorders, or premenstrual dysphoric disorder (PMDD). The menopausal transition is considered a “window of vulnerability” for depression, similar to puberty and the postpartum period. If you’ve experienced major depressive disorder at other hormone-sensitive times in your life, you’re at higher risk during this transition to menopause.
How long can menopause depression last?
Perimenopausal depression can last as long as the menopause transition itself, which averages about four years but can extend up to eight years. Most women experience perimenopause starting in the mid-to-late forties, though some women begin experiencing symptoms earlier. The transition of perimenopause ends with menopause when there is no menstrual cycle for 12 consecutive months.
For some women, depressive symptoms improve once hormones settle after menopause. Research indicates that promoting good mental health during the menopause transition through early intervention can reduce the duration and severity of depressive symptoms. However, without treatment, depression during perimenopause can persist into the postmenopausal years or become chronic. Perimenopausal and postmenopausal women both benefit from early intervention and appropriate treatment.
The timeline varies significantly based on:
- Whether you receive treatment and what type
- Your history of mood disorders
- Life circumstances and stress levels
- How severely hormonal changes affect you
- Whether you have other perimenopausal symptoms disrupting sleep
Getting better sleep can significantly impact mental health and help with symptoms of depression during perimenopause. Most women who address perimenopausal depression with appropriate treatment see improvement within weeks to months rather than waiting years for hormones to settle naturally.
What is the best supplement for perimenopause?
While supplements are widely marketed for perimenopause, the evidence for treating depression with supplements alone is limited. Some women find symptom relief from supplements like black cohosh for hot flashes or omega-3 fatty acids for general well-being. Still, these aren’t considered first-line treatments for perimenopausal depression or other mood disorders.
Research supports evidence-based treatments like therapy, lifestyle changes, and, when needed, antidepressants or hormone therapy rather than relying primarily on supplements. Most women see better results with comprehensive treatment approaches. If you’re considering supplements, discuss them with your primary care doctor or healthcare provider, as some can interact with medications or have health risks.
The most effective approaches to mental health during perimenopause are often non-pharmaceutical: regular exercise, stress reduction techniques, enough sleep, and staying socially connected. These lifestyle factors have strong research backing for improving mood disorders and overall well-being.
What helps with perimenopause and depression?
Multiple treatment approaches exist for managing depression during perimenopause, and combining strategies often works better than relying on one alone. Seeking support from a strong support system, including professionals and community groups, can significantly improve management of perimenopausal depression symptoms. Different women respond to different treatments, so working with your primary care doctor or mental health provider is essential.
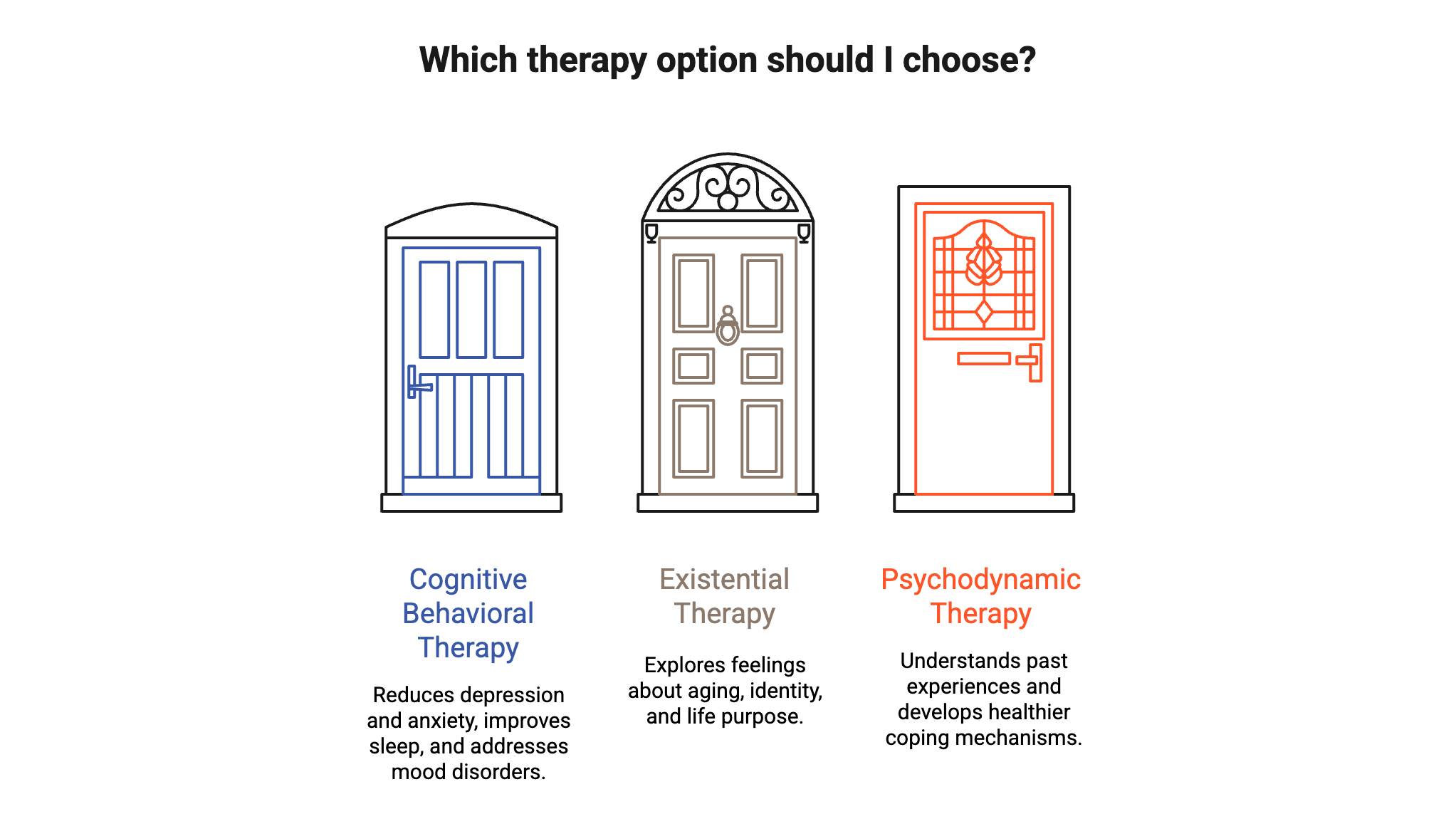
Therapy Options
Cognitive Behavioral Therapy helps reduce depression and anxiety during menopause by teaching you to identify and challenge negative thought patterns. CBT is proven to reduce depression and has the added benefit of helping with sleep problems and other symptoms during the menopausal stages. This evidence-based treatment can address both perimenopausal depression and other mood disorders.
For women grappling with bigger existential questions about aging, identity, and life purpose during this transition, existential therapy can be helpful. This approach helps you explore feelings about aging, loss, and finding meaning in new life stages—concerns that often surface during perimenopause.
Psychodynamic therapy looks at how past experiences and relationships affect your current feelings and behaviors. It helps you understand patterns in your life and develop healthier ways to cope with the emotional challenges of this life stage.
Lifestyle Changes and Self-Care
Lifestyle changes such as exercise and stress reduction can improve mental health during perimenopause. Regular exercise, limiting caffeine, and stress reduction techniques all contribute to better mood regulation. Exercise, healthy eating, and good sleep habits can improve mood and overall well-being even when hormonal fluctuations continue.
Getting enough sleep becomes especially important as women approach menopause. Create a cool sleeping environment to help with night sweats, establish consistent sleep and wake times, and address interrupted sleep as a priority rather than accepting it as inevitable. Lifestyle modifications, including regular exercise and socializing, can help reduce symptoms of perimenopausal depression and improve overall women’s health.
In our Dupont Circle practice, we work with many professional women balancing demanding careers with perimenopausal symptoms. What we find helpful is building a comprehensive mental health maintenance plan—regular therapy, consistent sleep habits, daily movement, and staying connected with friends. These aren’t optional extras during perimenopause; they’re essential infrastructure for getting through this transition with your wellbeing intact.
Medical Treatments
Antidepressants are commonly used to treat perimenopausal depression, particularly SSRIs and SNRIs. These medications can help with both depressive symptoms and some other symptoms like hot flashes. Treatment decisions should be made with your healthcare provider based on symptom severity and your individual health history.
Hormone therapy may relieve depressive symptoms associated with other perimenopausal symptoms, particularly if hot flashes are disrupting your sleep and contributing to mood problems. However, hormone replacement therapy is not typically recommended as a primary treatment for major depression. Menopause hormone therapy works best when depression is mild and clearly linked to other menopausal symptoms. Your doctor can help you understand if hormone therapy is appropriate for your situation.
When to seek help
If you’re struggling with mood changes that last more than two weeks or affect your daily life, don’t wait to see if they’ll resolve on their own. Regular communication with healthcare providers is essential for managing perimenopausal depression. Depression is a mental health condition that responds to treatment—it’s not a personal weakness or something you should simply endure. Getting help for depression during perimenopause can make a big difference in your quality of life.
Local resources like NAMI Washington DC provide information and support for individuals facing mental health challenges during perimenopause. The DC Department of Behavioral Health (DBH) also provides assessments, counseling, psychiatric evaluation, and medication management for mental health support.
Understanding the connection between perimenopause and depression helps you advocate for the care you need. This menopausal stage brings real physiological changes that impact your mental health, and recognizing when mood symptoms cross the line into depression empowers you to take action.
Get Support in Dupont Circle
If you’re in the DC area and struggling with mood changes during perimenopause, reach out to schedule an appointment with one of our therapists who understand the complex relationship between hormonal changes and mental health. You don’t have to face this transition alone.
Disclaimer: This blog provides general information about perimenopause and depression. It is not a substitute for professional medical or mental health advice, diagnosis, or treatment. If you are experiencing symptoms of depression or are in crisis, please contact your healthcare provider or call the National Suicide Prevention Lifeline at 988.