Tests for Depression: What to Expect and How They Work
If you’re wondering whether you might have depression, tests for depression can provide clarity. This guide is for anyone in Washington DC seeking to understand depression screening tools and what they reveal about mental health. You’ll learn about common assessment methods used by mental health professionals, what your results mean, and how to get appropriate care.
Depression screening uses brief questionnaires to identify potential depression and guide next steps. About 8% of U.S. adults experience depression, affecting millions of adults nationwide. Screening helps catch it early. These standardized tools (validated instruments that measure depressive symptoms) like the Patient Health Questionnaire-9 (PHQ-9—a 9-question screening tool) convert subjective feelings into numerical scores. Mental health professionals use these scores to measure symptom severity and track progress over time.
All positive screening results require additional assessment by a doctor or mental health professional to confirm major depressive disorder (a clinical diagnosis of persistent depression) and determine appropriate treatment. Screening is not the same as diagnosis—it’s the first step toward a full evaluation.
What is depression screening?
Depression screening is a brief questionnaire that identifies whether you might be experiencing depression. During routine medical visits, your doctor may ask you to complete a screening tool—usually taking just 2-5 minutes. The most common method is a self assessment form where you rate how often you’ve experienced specific symptoms over the past two weeks.
These aren’t diagnostic tests. Think of screening like a smoke detector—it alerts your doctor to check further, but doesn’t tell you exactly what’s wrong or how severe the problem is. A positive result simply means you need a more thorough evaluation.
In DC’s high-pressure environment, many people dismiss this as “just stress” or “burnout.” But when the feeling persists even during time off, or when you can’t identify a specific cause, it may signal clinical depression requiring assessment and treatment from a qualified mental health professional.
What is the PHQ-9 test for depression?
The Patient Health Questionnaire-9 (PHQ-9) is the most widely used and recommended test for depression screening. This 9-question self assessment questionnaire asks about depressive symptoms over the last two weeks. It covers sleep, interest in activities, energy levels, and mood changes. The Patient Health Questionnaire was developed for use in primary care settings. When you score 10 or higher, the PHQ-9 correctly identifies about 85% of people with depression.
Each question asks how often you’ve been bothered by symptoms like “little interest or pleasure in doing things” or “feeling depressed or hopeless.” The Patient Health Questionnaire was developed by Pfizer Inc and research institutions for primary care use.
Your total score indicates depression severity: 5-9 suggests mild symptoms, 10-14 indicates moderate depression, 15-19 signals moderately severe depression, and 20 or higher means severe depression requiring immediate care. The questionnaire takes just minutes to complete and is available at no cost. This is why it’s become the gold standard for screening across different healthcare settings.
Many people ask: what happens if I score positive on the PHQ-9? A positive score doesn’t mean you definitely have depression. It means you need a follow-up evaluation with your doctor or mental health professional.
At Therapy Group of DC, the Patient Health Questionnaire is part of our appointment making process. You’ll complete the PHQ-9, and your responses help us connect you with a therapist who specializes in what you’re experiencing—whether that’s depression, anxiety, or both.
What other screening tools exist?
Beyond the PHQ-9, mental health professionals may use other validated questionnaires. These include the Beck’s Depression Inventory-II (BDI-II—a 21-item self assessment questionnaire used to screen for depression), Center for Epidemiologic Studies Depression Scale (CES-D—designed for screening in general populations), Geriatric Depression Scale for older adults, or Edinburgh Postnatal Depression Scale (EPDS—designed for pregnant and postpartum women). Many depression assessment tools are available at no cost and have been validated for reliability and validity. Your doctor chooses based on your age and clinical context.
How do doctors test for depression beyond screening?
Once you’ve completed a screening questionnaire, the evaluation process goes deeper. Mental health professionals use a two-step approach: screening questionnaires followed by clinical interviews and physical exams. If your screening is positive, your doctor conducts a clinical interview. This gathers information about your symptoms and how they impact your life.
The interview assesses context that questionnaires can’t capture. This includes recent life stressors, your support system, past treatment, and whether symptoms are better explained by grief, medical conditions, or substance use. Doctors apply DSM-5 diagnostic criteria (the diagnostic manual for mental health) to determine if you meet the threshold for major depressive disorder. The diagnostic criteria for major depressive disorder require specific symptom patterns over a defined timeframe.
Physical exams and lab tests rule out medical issues like thyroid problems or vitamin deficiencies that can mimic depression symptoms.
We use a clinical interview at Therapy Group of DC to understand not just what symptoms you’re experiencing, but how they’re affecting your daily life. Are you avoiding social events? Struggling at work? Having trouble with relationships? These details help us recommend treatment that fits your situation.
What diagnostic criteria do doctors look for?
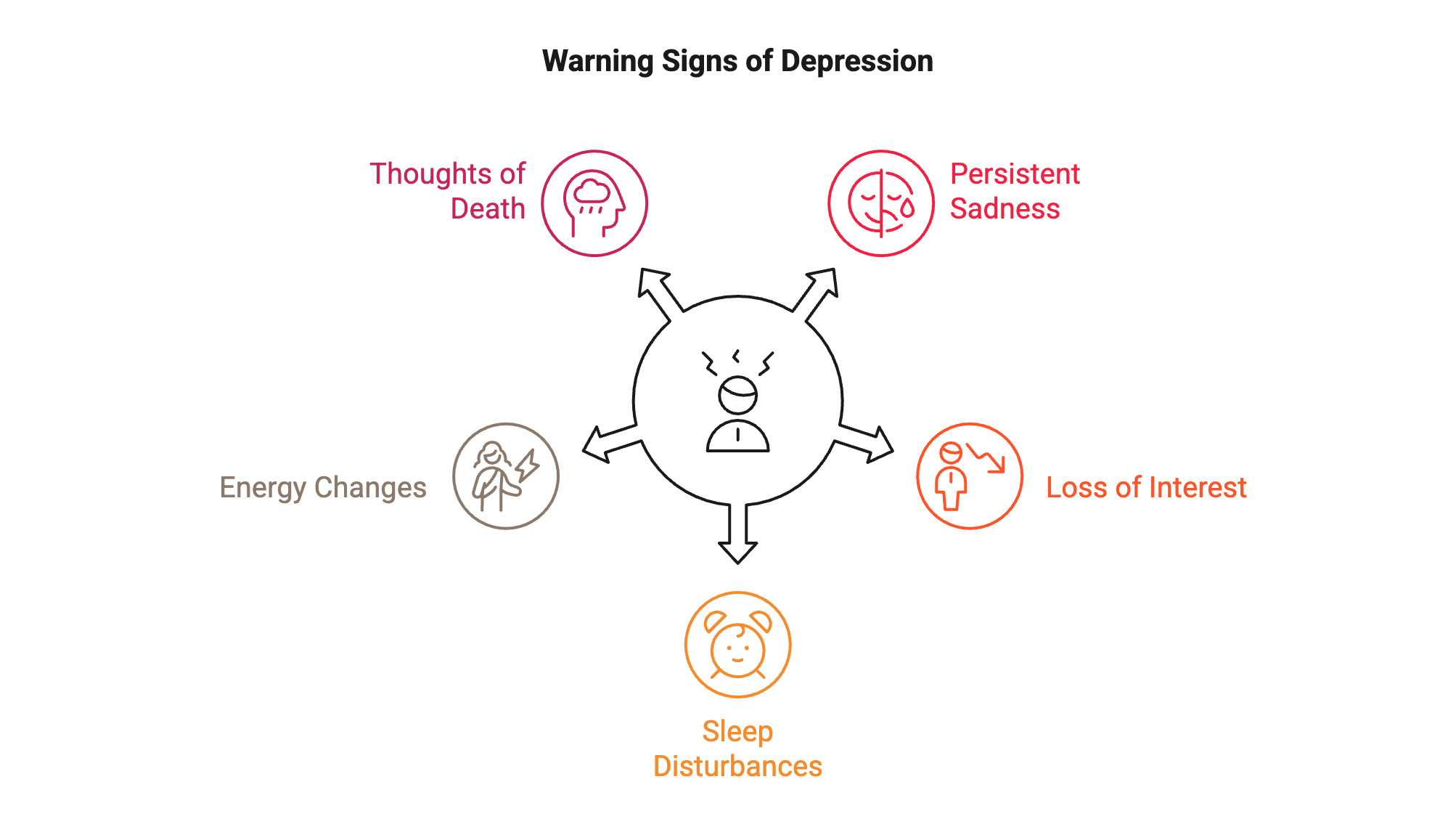
Doctors use the SIGECAPS framework (a memory tool) to assess depression symptoms: Sleep problems, Interest loss (little interest or pleasure in activities), Guilt or worthlessness, Energy depletion (feeling little energy or fatigue), Concentration difficulties, Appetite changes, Psychomotor changes, and Suicidal thoughts.
To diagnose major depressive disorder, doctors look for five or more symptoms during the same two-week period. At least one must be depressed mood or loss of interest. Symptoms must cause significant distress or interfere with daily functioning.
What about thoughts of suicide?
Any thoughts about being better off dead, hurting yourself, or suicide require immediate attention. These thoughts might be passive (“I wish I wouldn’t wake up”) or active (planning specific methods). The PHQ-9 specifically asks about this symptom because it signals severe depression and immediate risk. When combined with other symptoms like little energy, depressed or hopeless mood, or profound despair, these thoughts indicate you need urgent care.
If you’re experiencing thoughts of self harm, tell your doctor immediately or contact the 988 Suicide and Crisis Lifeline. This symptom indicates you need urgent care and safety planning, not just routine follow-up.
What happens after a positive screening?
After you’ve completed screening and discussed your symptoms, your doctor determines next steps. A positive screening result means you need additional assessment—it doesn’t automatically mean you have major depressive disorder. Moderate depression is common and treatable. Your mental health professional will:
- Confirm that symptoms meet diagnostic criteria (five or more SIGECAPS symptoms including depressed mood or loss of interest)
- Assess depression severity (how much symptoms interfere with daily life) to guide treatment planning
- Check for other mental health conditions like anxiety or bipolar disorder that can occur alongside depression
- Review your treatment history if you’ve been treated for depression before
- Conduct suicide risk assessment if you endorsed thoughts of death
Moderate depression and bipolar disorder both require evaluation by a mental health professional to ensure accurate diagnosis and appropriate treatment recommendations, whether that’s therapy, medication, or combined approaches.
How do I get help for depression in Washington DC?
If you’re wondering where to start after a depression diagnosis, you have several options. When you’re ready to address depression, working with a mental health professional makes a significant difference. Treatment typically involves therapy (especially cognitive behavioral therapy or interpersonal therapy). It may also include medication, or both, depending on symptom severity. Periodic assessment of depression helps gauge treatment progress and effectiveness.
Many people in Washington DC delay seeking help because they’re managing to function at work. But waiting for symptoms to become severe makes treatment harder and longer. Early intervention leads to faster improvement.
Your primary care doctor can provide referrals and, in many cases, prescribe antidepressant medication while connecting you with therapy. Understanding the difference between therapists and psychologists can help you find the right provider.
Ready to take the next step?
If you’re experiencing symptoms of depression, you don’t have to go through this alone. Therapy Group of DC offers d evidence-based mental health treatment with therapists in Dupont Circle.
Schedule an appointment to complete a thorough assessment and develop a personalized treatment plan. and offer evening and weekend appointments.
This blog provides general information and discussions about mental health and related subjects. The content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
CTA Text Suggestions:
- Header: Ready to Take the Next Step?
- Body: Schedule a consultation to discuss your symptoms
- Button: Contact Therapy Group of DC