What Is High-Functioning Depression? Symptoms, Treatment, and When to Seek Help
High-functioning depression describes people who experience symptoms of depression while still managing their daily responsibilities like work, relationships, and basic self-care. Unlike the stereotype of depression where someone can’t get out of bed, people with high-functioning depression may appear outwardly successful while quietly struggling with persistent sadness, low energy, and feelings of hopelessness. This term isn’t an official clinical diagnosis but rather describes a pattern seen in conditions like persistent depressive disorder and major depressive disorder.
This article is for individuals who suspect they may be dealing with high-functioning depression, their loved ones, and those seeking a deeper understanding of this often-overlooked condition. Recognizing high-functioning depression matters because individuals may suffer in silence while appearing outwardly successful.
What Is High-Functioning Depression?
High-functioning depression is an informal term used to describe individuals who maintain their functioning at work, school, or home despite experiencing significant depressive symptoms. The key feature is the disconnect between how someone appears externally and what they’re feeling internally. From the outside, everything looks fine. Internally, they’re dealing with chronic fatigue, poor concentration, and a persistent sense that nothing brings them joy.
Note that high-functioning depression is not an official clinical diagnosis in the DSM-5.
This pattern can occur with different clinical diagnoses. Persistent depressive disorder, also known as dysthymia, is a chronic form of depression lasting at least two years. It often presents with this high-functioning pattern, as people learn to adapt to low-level depressive symptoms over time. Research shows that persistent depressive disorder can be chronic and disabling despite appearing less severe on the surface.
Individuals with high-functioning depression may experience persistent depressive disorder (PDD), marked by constant fatigue and a lack of energy.
High-functioning depression can also describe someone with major depressive disorder who continues working and fulfilling obligations despite meeting criteria for clinical depression. The Diagnostic and Statistical Manual doesn’t include “high-functioning” as a severity specifier, but mental health professionals recognize this presentation as common and serious—particularly among successful professionals who’ve learned to mask their struggles.
In our practice, we regularly see high achievers in DC who’ve been functioning with depression for years without realizing it. They assume depression means you can’t work, but that’s not always true. Recognizing that you can be both successful and struggling is often the first step toward getting help.
What Are the Symptoms of High-Functioning Depression?
The symptoms of high-functioning depression mirror those of other depressive disorders but occur while the person maintains daily functioning. Common signs include both emotional and physical changes that persist for weeks or months.
Emotional symptoms:
- Persistent sadness or feelings of emptiness
- Loss of interest in activities you once enjoyed
- Feelings of hopelessness about the future
- Low self-esteem and harsh self-criticism
Physical symptoms:
- Low energy and fatigue that rest doesn’t fix
- Sleep disturbances (sleeping too much or too little)
- Changes in appetite or weight
- Physical aches without clear medical cause
Cognitive symptoms:
- Poor concentration and difficulty focusing on tasks
- Difficulty making decisions, even minor ones
- Negative self-talk and excessive self-criticism
- Thoughts that life isn’t worth living
Behavioral symptoms show up in how you cope with depression. Many people with high-functioning depression rely heavily on routines to get through the day, withdraw from social situations despite maintaining necessary obligations, and use work or achievement to mask their struggles. In a city where career identity runs deep, using professional success to hide depression is particularly common.
Research shows that preserving functionality despite severe depressive symptoms can actually be a protective factor that predicts better outcomes when people do seek treatment.
We often hear from clients that they didn’t recognize their symptoms as depression because they were still performing well at work. The disconnect between external functioning and internal suffering can persist for years. Many people come to therapy only when a major life event finally overwhelms their coping strategies.
How Is High-Functioning Depression Different from Major Depression?
The main difference isn’t in the symptoms themselves but in how they affect daily life and how visible they are to others. Someone with high-functioning depression continues meeting their responsibilities despite significant distress, while someone with more severe major depressive disorder may be unable to work or care for themselves.
This doesn’t mean high-functioning depression is less serious or worthy of treatment. The chronic stress of maintaining appearances while struggling internally often leads to:
- Burnout and worsening symptoms over time
- Strained relationships with family and friends
- Increased risk of other mental health conditions like anxiety
- Progressive decline in well-being
The severity of clinical depression exists on a spectrum. Depression can be mild, moderate, or severe, and someone can function well with moderate depression while another person with similar symptom severity cannot. How much depression impacts your functioning depends on many factors including the duration of symptoms, available support systems, workplace flexibility, and coping skills developed over time.
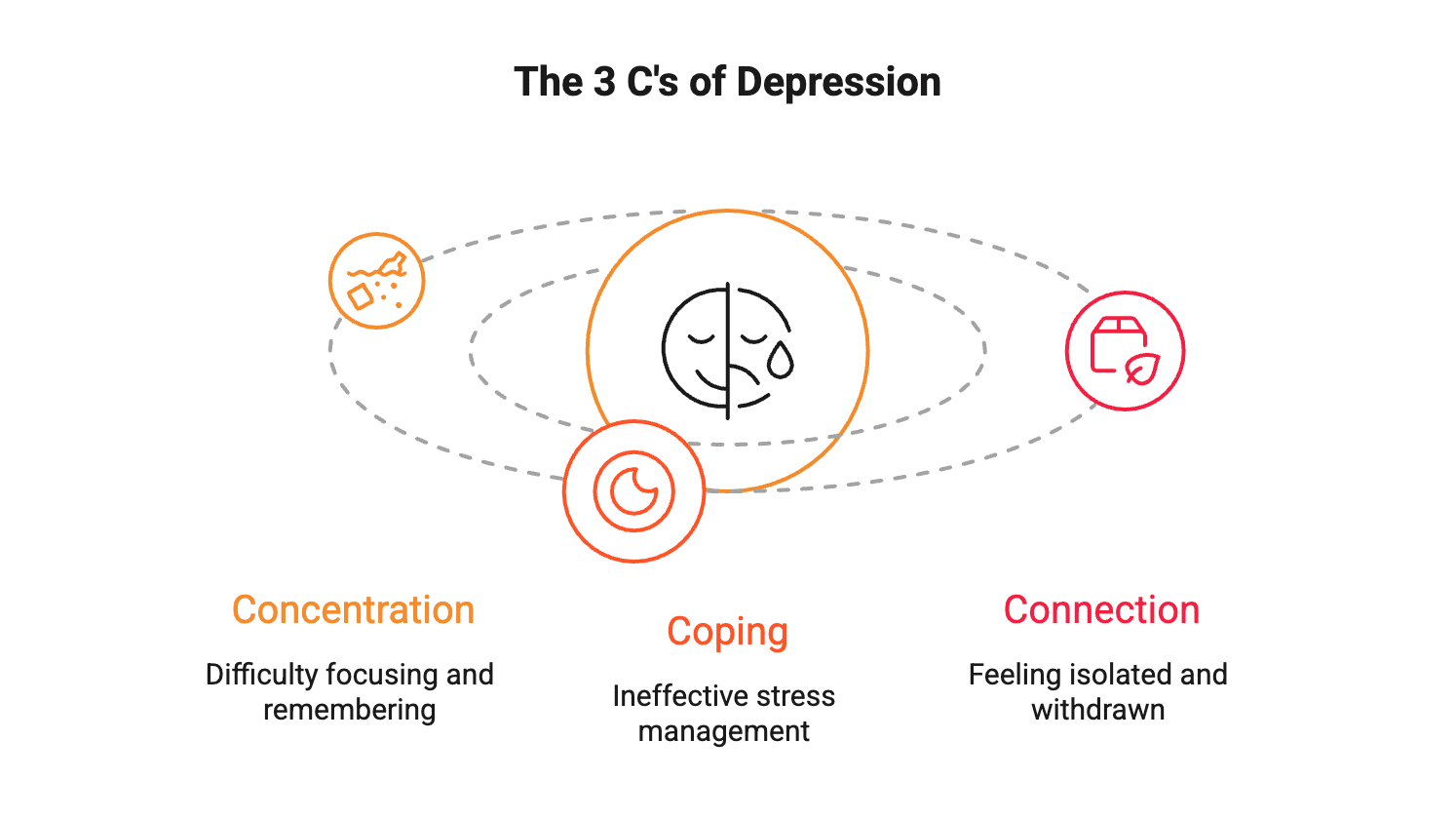
What Are the 3 C’s of Depression?
While “the 3 C’s” isn’t a universally standardized clinical framework, mental health professionals often discuss three core areas affected by depression:
Concentration — Depression significantly affects cognitive functioning. You might struggle to focus on tasks, make decisions, or remember information. This is why even high-functioning individuals with depression often feel like they’re working twice as hard to achieve the same results.
Coping — Depression affects your ability to manage stress and regulate emotions. Coping skills that used to work may no longer be effective. People with high-functioning depression frequently develop maladaptive coping strategies like overworking, emotional suppression, or perfectionism to compensate for how they’re feeling.
Connection — Depression impacts relationships and your sense of connection to others. You might withdraw from friends and family, feel isolated even in crowds, or struggle to feel emotionally close to people who care about you. Maintaining social connections becomes exhausting when you’re constantly masking how you really feel. Relationship difficulties can both contribute to and result from depression.
What Treatment Options Are Available for High-Functioning Depression?
Effective treatment for high-functioning depression typically involves psychotherapy, medication, or a combination of both approaches. Research shows that psychotherapy is a proven first-line treatment for depression, with approximately 50% of people responding to therapy compared to 25% without treatment.
Psychotherapy Approaches
There are several evidence-based therapy options, and different types of therapy can be equally effective depending on your preferences and needs.
Cognitive Behavioral Therapy (CBT) helps you identify and change negative thought patterns affecting your mood. This is particularly helpful for high-functioning depression because it addresses the perfectionism and harsh self-criticism that often fuel the condition.
Interpersonal Therapy focuses on improving relationships and communication patterns. This approach can help you stop masking your struggles and build more authentic connections with others.
Psychodynamic therapy explores how past experiences and unconscious patterns influence current feelings. Many high achievers benefit from understanding the deeper patterns that drive their need to maintain appearances despite struggling. This therapeutic approach offers insights into recurring relationship dynamics and emotional conflicts.
Behavioral Activation focuses on increasing positive activities and engagement with life, which can be especially effective when depression has made everything feel pointless.
No single therapy type has proven better than others for most people, so personal preference matters when choosing your approach.
Medication Options
Antidepressant medication can be highly effective for persistent depressive disorder and major depressive disorder. SSRIs and SNRIs are commonly prescribed first-line medications often used in combination with therapy for better outcomes.
For treatment-resistant depression that doesn’t respond to standard approaches, other options may include medication combinations, different classes of antidepressants, or newer treatments like ketamine-assisted psychotherapy or transcranial magnetic stimulation (TMS).
Lifestyle Changes
While not replacements for professional treatment, certain lifestyle changes can enhance your mental health outcomes:
- Structured exercise has been shown to improve mood
- Improved sleep hygiene helps regulate brain function and emotion
- Reducing alcohol use prevents worsening of depressive symptoms
When Should You Seek Professional Help?
You don’t need to wait until you “can’t function” to seek treatment. If depressive symptoms have lasted more than two weeks and are causing you significant distress, it’s time to talk with a healthcare provider or licensed clinical psychologist.
Seek help immediately if you experience:
- Thoughts of self-harm or suicide
- Increasing hopelessness or feeling trapped
- Significant difficulty taking care of basic needs
- Substance use to cope with feelings
Many people with high-functioning depression wait years before seeking support because they believe their struggles aren’t “serious enough.” This is a misconception. The fact that you’re managing to function doesn’t mean you’re not suffering or that you don’t deserve support. Depression is a medical condition, not a character flaw or a sign of weakness.
Treatment doesn’t mean admitting defeat. It means choosing to feel better and recognizing that living with chronic emotional pain isn’t a badge of honor—it’s unnecessary suffering when effective treatments exist.
In our DC practice, we specialize in working with professionals who are used to handling everything themselves. The hardest part is often acknowledging you need support. We’ve seen countless clients improve dramatically once they take that first step, even those who’ve been functioning with depression for years.
If you’re concerned about a family member or friend, encourage open conversations about mental health. Let them know that their struggles are valid regardless of how well they appear to be coping. Sometimes recognizing that someone else sees what you’re dealing with can be the nudge someone needs to seek treatment.
Get Support for Depression in DC
If you’re experiencing signs of high-functioning depression, the Therapy Group of DC can help. Our licensed clinical psychologists and therapists specialize in treating persistent depressive disorder, major depression, anxiety, and the unique challenges facing high-achieving professionals in Washington, DC.
Connect with our depression specialists to schedule a consultation and begin your path toward feeling better.
This blog provides general information and discussions about mental health and related subjects. The content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
Frequently Asked Questions About High-Functioning Depression’
How Can I Support Someone with High-Functioning Depression?
If you’re concerned about someone who seems to be struggling despite appearing fine, encouraging open conversations about mental health is crucial. Let them know it’s okay to seek support regardless of how well they seem to be handling things on the surface. Avoid minimizing their experience by saying they’re “just stressed” or “too successful to be depressed.” Your compassion and recognition of their struggles—even when they’re not obvious—can be the nudge someone needs to seek professional help.
Can High-Functioning Depression Get Worse Over Time?
Yes, untreated high-functioning depression often worsens. The longer depression goes unaddressed, the more entrenched symptoms become. Research shows that untreated major depressive disorder may result in progressive alterations in brain structure and function. Chronic emotional suppression and stress from maintaining appearances can lead to severe burnout, worsening mental health, physical health problems, and increased risk of major depressive episodes. Evidence shows that a delay in treatment is associated with poorer clinical outcomes, underscoring the importance of early intervention.
Is High-Functioning Depression the Same as Being “Stressed”?
No. While stress is a normal reaction to challenging situations that typically improves when circumstances change, high-functioning depression involves persistent depressive symptoms lasting weeks, months, or years. Depression affects brain chemistry, mood regulation, and daily functioning in ways that stress management alone cannot fix. If you’ve felt persistently sad, empty, or hopeless for more than two weeks despite managing your responsibilities, you’re likely dealing with depression—not just stress.