When Your Body Changes But Your Relationship Doesn’t: Navigating Sex Drive During Menopause
Query Confirmation: Menopause and Sex Drive
Menopause can lead to a significant decline in sexual desire for some women, while others may experience an increase or no change at all. This guide is for women in Washington DC experiencing changes in their sex life during menopause. You’ll learn how physical symptoms affect intimacy, why relationship dynamics matter, and when couples therapy can help.
Changes in sexual desire during menopause are common. While decreasing hormone levels play a role, physical symptoms often create anxiety about sex and strain partner communication. Research shows that sexual concerns involve multiple factors—biological, psychological, and relationship dynamics—which is why the most effective treatment often combines different approaches.
How Does Menopause Affect Your Sex Life?
The sexual response cycle can be affected during menopause, leading to changes in libido, arousal, and orgasm. Perimenopause—the transition period that can begin 8 to 10 years before your final menstrual period—is often associated with changes in sexual desire.
Low estrogen levels during menopause can lead to vaginal dryness, which may make sex uncomfortable and reduce sexual desire. Common menopausal symptoms such as hot flashes, night sweats, and mood changes can contribute to a lower sex drive.
Vaginal dryness and discomfort during sex create anxiety about intimacy, which further reduces desire and satisfaction. This becomes a cycle—physical discomfort leads to avoiding sex, which increases relationship tension.
In our DC practice, we see women who excel at managing high-pressure careers but feel lost when their bodies change. The skills that help you navigate work challenges—clear communication, problem-solving, seeking expert help—can also help you navigate changes in your sex life.
Why Decreased Sexual Desire Creates Relationship Tension
Low sex drive can lead to conflicts and strife in relationships. When one partner’s sexual interest changes significantly during menopause while the other’s stays the same, this creates a disconnect that affects more than just physical intimacy.
Your partner may interpret your decreased interest as rejection or loss of attraction, even when the real cause is vaginal atrophy, painful intercourse, or exhaustion from managing menopausal symptoms. You might feel pressure to have sex when you’re not interested, or guilt about “not being enough.” These feelings strain communication and create emotional distance.
Changes in mental health and self-esteem can also impact sexual desire. Poor body image and increased stress contribute to lower libido—especially when caring for aging or ill parents while managing your own transition.
When Physical Symptoms Make You Avoid Intimacy
Vaginal dryness and shrinking of the vagina are common symptoms of menopause that can make sex uncomfortable. Low estrogen levels reduce natural lubrication in the vagina, leading to discomfort during sex. This is called dyspareunia (painful sex), and it significantly impacts whether you want to be sexually active.
Painful intercourse creates a psychological barrier. If sex has hurt several times, the reproductive system starts to tense up in anticipation, making arousal difficult. This response is normal—your body is trying to protect you.
Good news: many sexual problems can be successfully treated. Vaginal lubricants provide short-term relief. Vaginal moisturizers maintain tissue health long-term. Some women benefit from hormone therapy to address low sex drive and improve comfort during sex.
What Actually Helps With Physical Symptoms
Effective treatments for vaginal dryness include:
- Vaginal lubricants – Applied before sexual activity for immediate relief
- Vaginal moisturizers – Used 2-3 times weekly to maintain vaginal tissue health
- Low-dose vaginal estrogen – Restores tissue elasticity with minimal systemic absorption
- Hormone replacement therapy – Relieves symptoms of genitourinary syndrome (GSM)
Pelvic floor exercises strengthen supportive muscles and improve blood flow to the pelvic region, which can enhance sexual arousal.
The Mental Health Impact: Anxiety About Sex, Body Image, and Depression
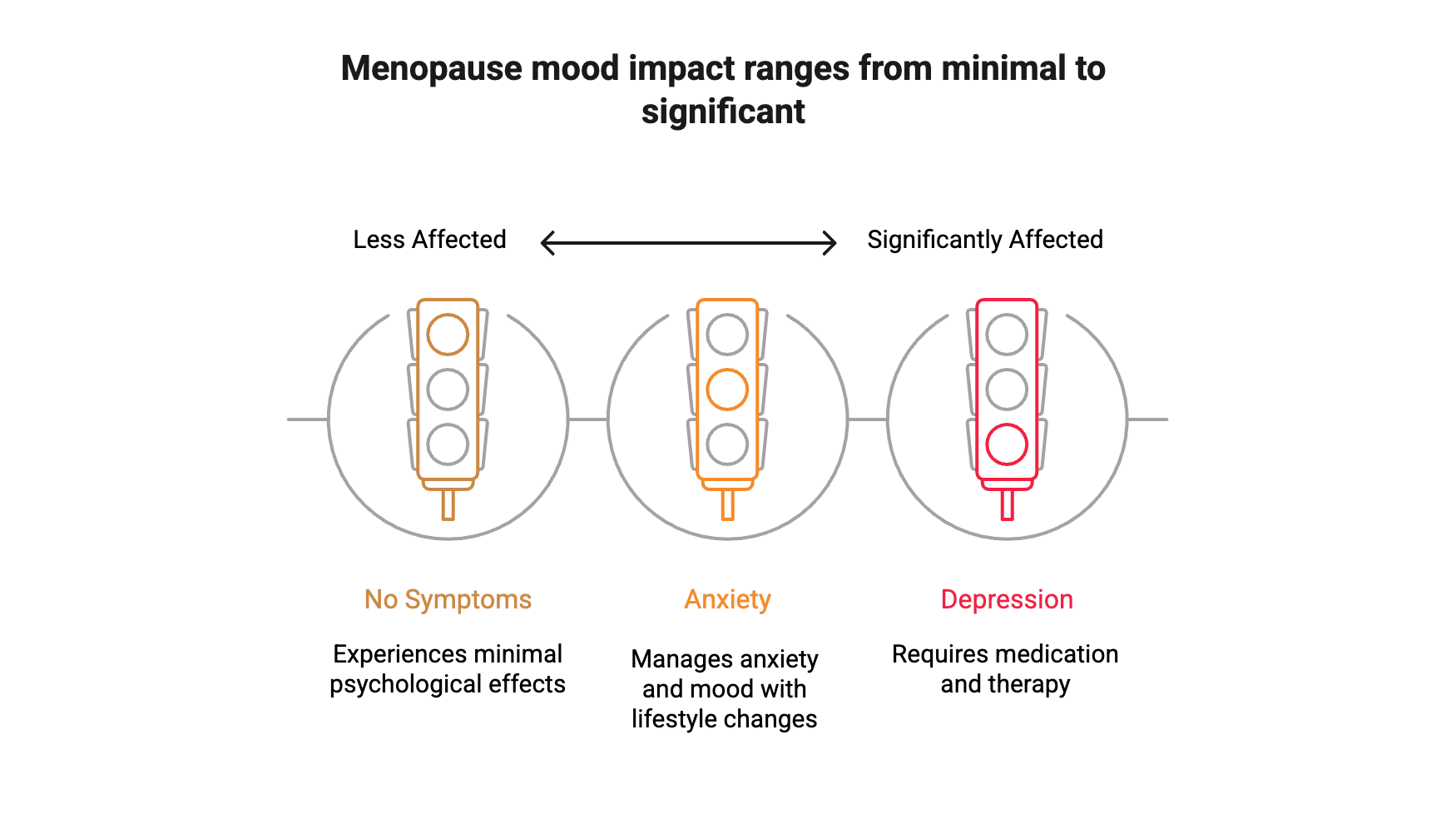
The connection between menopause and mood is complex. Not all women experience psychological symptoms during menopause. You are not universally at risk for anxiety or depression just because you’re going through this transition.
Certain factors increase risk: severe hot flashes and night sweats that disrupt sleep, stressful life events happening simultaneously (like adult children living at home or caring for ill parents), and a history of depression.
Anxiety disorders can reduce sexual interest during menopause. When managing anxiety about work, aging, and bodily changes, adding sexual performance pressure creates overwhelm. Depression and low sexual desire create a vicious cycle—depression reduces interest in pleasurable activities, including sex, and loss of sexual connection can deepen depression.
Some women experience lower libido due to medications, such as selective serotonin reuptake inhibitors (SSRIs), commonly prescribed to treat depression. If a medication is lowering your sex drive, do not stop taking it without talking to a healthcare professional first. Your provider can adjust medications or suggest alternatives.
In our practice, we see women caught between managing their mental health and maintaining their sex life. Good news: you don’t have to choose. Working collaboratively with both your therapist and prescriber, we can find solutions that support both.
Weight gain, another hallmark symptom, affects body image and contributes to lower sexual confidence.
How to Talk With Your Partner About Changes in Sexual Interest
Open communication with your partner about sexual health concerns can enhance intimacy and satisfaction. This conversation doesn’t come naturally for most couples.
Here’s how to start: Name what’s actually happening—”I want to be close to you, but sex has been painful because of vaginal dryness,” or “My hot flashes leave me exhausted by evening, which affects my interest in sex.” This separates the physical reality from your feelings about your partner.
Relationship quality affects intimacy significantly during menopause. Communication difficulties and relationship stress can all affect intimacy. Many women find that addressing these relationship issues is just as important as treating physical symptoms.
Exploring new forms of intimacy beyond intercourse—such as massage or physical affection—can help maintain connection with your partner during menopause. You can have a fulfilling sex life that looks different than before.
When Couples Counseling Helps Restore Intimacy
Therapy helps sexual concerns effectively. Sex therapy and couples counseling should be considered important options for care.
Consider couples therapy when:
- Communication about sex and intimacy has become difficult
- Relationship stress is affecting your sex life
- You and your partner have different expectations around sexual activity
- One partner feels rejected while the other feels pressured
Counseling significantly improves sexual function in postmenopausal women. These programs typically include 4-10 sessions covering sexual anatomy, how the body responds during sex, understanding menopause-related changes, and addressing common myths about sex and aging.
Some approaches incorporate mindfulness techniques to help you stay present and reduce anxiety during intimate moments. Cognitive-behavioral therapy techniques help identify and change unhelpful thought patterns about sex and menopause.
We work with couples where both partners are high-achieving professionals used to solving problems quickly. Sexual concerns during menopause require a different approach—one that’s more collaborative, experimental, and patient. Therapy provides the framework for that shift.
Does Your Sex Drive Return After Menopause?
Many postmenopausal women can maintain or even improve their sex lives after the transition period ends. The answer depends on multiple factors: how physical symptoms are managed, mental health treatment if needed, relationship quality, and whether sexual concerns cause distress.
Some women experience renewed interest in sex once they’re no longer worried about pregnancy and after their menstrual periods stop. Others find that once menopausal symptoms stabilize and they’ve adapted to physical changes, sexual desire returns—though it may feel different than before.
For some women, hormone levels eventually stabilize at a lower level, and the body adjusts. Lifestyle changes—regular exercise, stress management, adequate sleep, maintaining a healthy diet—can make a big difference in your desire for sex by improving overall well-being and energy.
The question isn’t necessarily “Will my old sex drive return?” but rather “Can I develop a satisfying sex life that fits who I am now?” For most women, the answer is yes, with the right combination of physical treatment, psychological support, and relationship work.
Ready to Get Support?
Talking about sexual concerns can feel uncomfortable, but healthcare professionals are trained to discuss these issues. Many women find that once they start the conversation, they feel relieved and empowered to seek help.
If you’re experiencing distress related to sexual changes during menopause, consider talking with your primary care provider or gynecologist, asking for a referral to a sex therapist or couples counselor, or connecting with our DC therapists who specialize in individual therapy for women’s mental health and relationship concerns.
Sexual well-being is an important part of overall health and quality of life. Seeking help for sexual concerns is a valid and important step in caring for yourself during the menopause transition and beyond.
This blog provides general information and discussions about mental health and related subjects. The content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.