Will Depression Make You Tired? Understanding When Exhaustion Signals Something More
Feeling tired all the time can be frustrating, especially when rest doesn’t seem to help. You might wonder if something deeper is going on—and you’re right to pay attention. Depression can cause severe fatigue that feels different from ordinary tiredness, affecting more than 90 percent of people with major depressive disorder. More than 90 percent of patients experience severe fatigue as part of their depression symptoms, making exhaustion one of the most common signs something is affecting your mental health.
Unlike the tiredness you feel after a long day, depression fatigue doesn’t improve with sleep. It makes simple tasks feel overwhelming and creates a cycle that’s hard to break without professional help. If you’ve been dragging through your days in Dupont Circle or elsewhere in DC, understanding the connection between depression and exhaustion is an important first step toward treating depression effectively.
Is Tiredness a Symptom of Depression?
Yes, fatigue is one of the most prevalent symptoms of major depressive disorder. Fatigue impacts physical, cognitive, and emotional functions in people experiencing clinical depression, making it a core symptom rather than just a side effect.
Depression fatigue shows up differently than normal tiredness. While regular exhaustion improves with rest, depression-related fatigue persists even after sleeping. Many people describe it as feeling physically heavy, mentally foggy, or completely drained of motivation. This exhaustion affects your ability to concentrate, make decisions, or engage in activities you once enjoyed—impacting both your mental health and physical health.
The fatigue associated with depression often appears alongside other symptoms like low mood, changes in appetite, sleep problems, and difficulty concentrating. When these symptoms cluster together, they signal your tiredness might be more than needing a vacation—it could be depression impacts on your brain chemistry and stress response system.
In our practice, we often hear clients describe depression fatigue as fundamentally different from regular tiredness—being “tired in my bones.” They’re frustrated that rest doesn’t help and often blame themselves for not being able to “push through.” We help clients understand that this exhaustion is a biological symptom, not a character flaw. Recognizing it as part of depression rather than personal weakness is often the first step toward self-compassion and seeking appropriate treatment.
What Are the Symptoms of Severe Depression?
Severe depression involves multiple symptoms that significantly interfere with daily life, not just feeling sad. The depressive symptoms can include different symptoms that affect your mood, body, and thinking:
- Persistent low mood or feelings of emptiness
- Loss of interest in activities you used to enjoy
- Severe fatigue that doesn’t improve with rest
- Sleep problems (insomnia or excessive sleeping)
- Changes in appetite or weight
- Difficulty concentrating or making decisions
- Feelings of worthlessness or excessive guilt
- Physical symptoms like muscle aches and pains
- Mood swings or irritability
- Thoughts of death or self-harm
Depression can cause fatigue that makes these other symptoms worse. When exhaustion is severe, it diminishes your motivation to engage in social activities, exercise, or other behaviors that might improve your mental health. This creates a challenging cycle where depression causes fatigue, and fatigue makes depression harder to manage.
Why Does Depression Make You So Tired?
Depression disrupts brain chemistry and the body’s stress response, leading to persistent exhaustion. Several factors contribute to this connection, creating what researchers call a “biopsychosocial” impact on energy.
Your brain’s chemical messengers—including serotonin and dopamine—help regulate both mood and energy. When depression affects these neurotransmitters, your brain struggles to maintain normal energy levels. Low dopamine levels are associated with fatigue and lack of motivation, while serotonin dysregulation impacts sleep quality and energy. This brain chemistry imbalance affects how your body processes energy and manages rest.
The body’s stress response system can become overactive in depression. High cortisol levels from chronic stress keep your body in a state of alert exhaustion, burning through energy reserves without providing actual rest. This creates a paradox where you’re simultaneously wired and depleted—a common experience in severe depression.
Research suggests that inflammation may also contribute to feelings of fatigue in depression, making your whole body feel run down. This biological response affects everything from your immune system to your ability to recover from daily activities.
Sleep disturbances compound the problem. Even if you spend hours in bed, depression can lower sleep quality, leaving you without the restorative rest your brain and body need. You might struggle with insomnia, wake frequently during the night, or sleep excessively without feeling refreshed—all common sleep problems in mental health conditions like depression.
We consistently see how depression fatigue creates a trap: clients feel too exhausted to do the things that might help them feel better—exercise, socializing, or even attending therapy appointments. In our work, we start where clients are rather than where they “should” be. If getting to the gym feels impossible, we might begin with standing up and stretching for two minutes. Small wins matter because they prove that movement is possible, which challenges the depression narrative that nothing will help.
What to Do When You’re Too Depressed to Do Anything?
Start with the smallest possible step and reach out for professional help. When depression fatigue makes everything feel impossible, trying to overhaul your entire life at once backfires. Instead, focus on tiny, manageable actions that help you cope with the immediate challenge.
Begin by talking to a doctor. They can help determine if your fatigue is due to depression, a medical condition, medication side effects, or multiple factors. Treating depression often improves energy levels, but you need an accurate understanding of what’s happening first. Your healthcare provider can discuss options including therapy, lifestyle changes, and when appropriate, antidepressant medication.
Strategies to Support Your Recovery
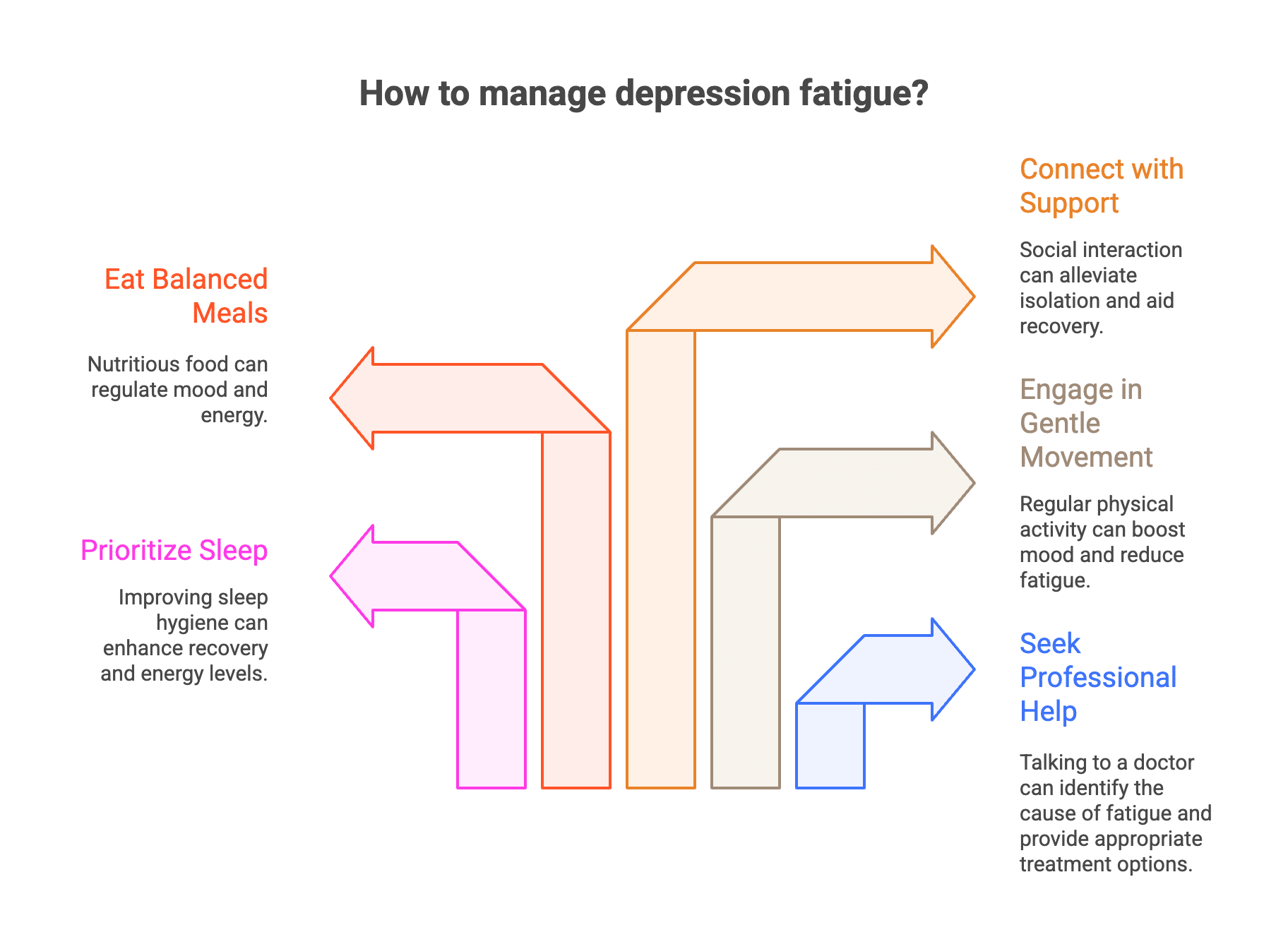
While professional treatment is essential, some approaches can help reduce fatigue and support your overall recovery:
Prioritize sleep. Practice good sleep hygiene by keeping a consistent sleep schedule, limiting screens before bed, and creating a calm bedroom environment. Better sleep won’t cure depression, but it can help promote quality sleep that supports recovery.
Move your body gently. Start with just five minutes of gentle movement—a short walk, stretching, or dancing to one song. Regular physical activity can alleviate fatigue over time by releasing mood-boosting chemicals in your brain.
Eat balanced meals. Focus on whole grains, lean proteins, and vegetables to help regulate mood and energy naturally. Limit processed foods and added sugars that create energy crashes.
Connect with support. Whether through loved ones or talking therapies, connection matters. Isolation intensifies depression and makes managing fatigue harder.
When Should I Go to the Hospital for Depression?
Seek emergency care immediately if you have thoughts of harming yourself or others. This is a medical emergency requiring urgent attention. Go to your nearest emergency room or call 911.
If you’re experiencing thoughts of self-harm but aren’t in immediate danger, call 988 (the Suicide and Crisis Lifeline) to speak with trained counselors who can provide support and connect you with resources.
Other situations that warrant urgent evaluation include:
- Inability to care for yourself or complete basic self-care
- Severe symptoms that prevent you from functioning
- Rapid worsening of depression or emergence of psychotic symptoms
- Concern from family members or loved ones about your safety
Depression is treatable, but severe cases require immediate professional intervention. Don’t wait until you’re in crisis—early treatment prevents complications and helps you feel better faster.
Treatment Options That Work
Multiple evidence-based treatments effectively address both depression and fatigue. Management of depression in adults typically involves therapy, lifestyle modifications, and sometimes medication to treat the full range of symptoms.
Talking therapies like cognitive-behavioral therapy (CBT) help you identify and change thought patterns that maintain depression. These approaches teach coping methods for managing symptoms and breaking the cycle of depression fatigue. Other effective talking therapies include interpersonal therapy, which focuses on relationship patterns, and mindfulness-based approaches that help you cope with difficult feelings.
For some people, antidepressant medication helps restore brain chemistry balance. Some medications may cause initial fatigue as a side effect, while others are generally better tolerated. Your doctor can help find the right medication if needed, and switching options is always possible if side effects become problematic.
Treating residual symptoms is important. Even after depression improves, some people continue experiencing fatigue or other lingering symptoms. Working with your treatment team to address these residual symptoms ensures more complete recovery and reduces the risk of depression returning.
Find Support for Depression in DC
If you’re looking for support with depression and fatigue, the therapists at Therapy Group of DC are here to help. We understand how exhausting it is to fight through every day when depression makes you tired, and we offer evidence-based talk therapy to address the root causes. Schedule an appointment to get started.
Frequently Asked Questions About Depression and Fatigue
Can depression cause trouble falling asleep and staying asleep?
Yes, depression often disrupts normal sleep patterns, leading to trouble falling asleep and staying asleep. These sleep problems reduce quality sleep, contributing to persistent fatigue and making it harder to manage depression fatigue effectively.
How can moderate intensity exercise help with depression fatigue?
Engaging in moderate intensity exercise regularly can increase energy levels and reduce feelings of fatigue. Exercise promotes quality sleep and releases mood-regulating neurotransmitters, helping to break the cycle of exhaustion commonly experienced in major depressive disorder.
Are there specific medications that can treat fatigue associated with depression?
Certain antidepressants like bupropion are associated with lower levels of residual fatigue compared to others such as tricyclic antidepressants. Additionally, adjunctive treatments and psychostimulants may be used to specifically treat fatigue symptoms in patients with depression. Consult a psychiatrist or a psychiatric-mental health nurse practitioner (PMHNP) about this.
Disclaimer: This article is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or qualified mental health provider with any questions you may have regarding a medical or mental health condition. If you are in crisis or experiencing thoughts of self-harm, please call 988 (Suicide and Crisis Lifeline) or go to your nearest emergency room.