What Are the Strengths and Weaknesses of Cognitive Behavioral Therapy?
Cognitive behavioral therapy CBT is one of the most researched and effective forms of psychotherapy available, with strong evidence from number studies supporting its use for depression, anxiety disorders, post traumatic stress disorder, obsessive compulsive disorder, and eating disorders. Comprehensive research consistently shows that cognitive behavioral therapy CBT helps most people experience meaningful symptom improvement, often performing as well as medication and sometimes offering superior long-term benefits.
However, like any therapeutic approach, cognitive behavioral therapy has both strengths of cognitive behavioral therapy and limitations that are important to understand when considering treatment options for mental health conditions.
What Are the Main Strengths of Cognitive Behavioral Therapy?
Cognitive behavioral therapy CBT offers several distinct advantages that make it the best therapy for anxiety and a preferred first-line treatment for many mental health conditions. Research demonstrates that cognitive behavioral therapy CBT produces substantial improvements across a wide range of mental health conditions. Multiple studies and meta analyses reveal effect sizes that rival or exceed pharmacological treatments for depression and anxiety disorders.
One of the primary strengths of behavioral therapy is its focus on teaching practical, transferable skills. Rather than simply providing symptom relief during therapy sessions, cognitive behavioral therapy CBT empowers individuals to identify and challenge negative thoughts and negative emotions, develop effective coping skills for emotional regulation, and build behavioral techniques they can use independently. CBT helps people in their daily life long after treatment ends. In DC where high-achieving professionals face constant pressure, these portable skills for managing own mental health become especially valuable.
Another significant advantage is the time-limited structure of cognitive behavioral therapy. Most people complete cognitive behavioral therapy CBT in 8 to 20 therapy sessions, making it one of the more focused and efficient therapeutic approaches for mental health conditions. This brief timeline appeals to clients who want clear treatment goals and measurable progress.
Cognitive behavioral therapy CBT also demonstrates remarkable versatility in delivery. Beyond traditional in-person therapy sessions, behavioral therapy works effectively through online platforms, group formats, and guided self-help programs. This flexibility enhances access for people with scheduling constraints, mobility limitations, or limited mental health professionals in their area.
In our practice at Therapy Group of DC, we consistently see clients benefit from cognitive behavioral therapy’s structured, skill-focused approach. We find that the collaborative nature of cognitive behavioral therapy CBT—where a CBT therapist and client work together to identify problems and test solutions—resonates particularly well with analytically-minded professionals who appreciate having concrete CBT techniques and homework assignments between therapy sessions. This active, goal-directed format works especially well for individuals who thrive with clear frameworks and measurable progress markers.
The evidence base supporting cognitive behavioral therapy CBT is another key strength. Comprehensive meta analyses spanning hundreds of randomized controlled trials and clinical trials confirm the effectiveness of cognitive behavioral therapy CBT across diverse populations, age groups, and clinical practice settings. These meta analyses in clinical psychology give both mental health professionals and clients confidence in the cognitive therapy approach.
Does CBT Provide Long-Term Benefits?
Perhaps one of cognitive behavioral therapy’s most compelling strengths is its durability. Multiple meta analyses—comprehensive reviews combining results from many studies—tracking patients for years after completing cognitive behavioral therapy CBT show that many people maintain their therapeutic gains. These research reviews provide particularly strong evidence for sustained improvement in anxiety disorders and depression. Relapse rates remain relatively low—typically between 0-14% within the first year—especially when clients continue practicing the coping skills and emotional regulation techniques they learned in therapy sessions.
What Are the Limitations and Weaknesses of CBT?
While highly effective for many mental health conditions, cognitive behavioral therapy CBT is not universally successful and comes with important limitations that deserve honest consideration. Understanding these weaknesses, documented across many meta analyses, helps set realistic expectations and identify who might benefit from other therapies or additional therapeutic approaches.
Meta analyses indicate that approximately one in four people who try cognitive behavioral therapy CBT do not achieve sufficient symptom relief from CBT treatment alone. This response rate varies depending on the specific mental health condition, symptom severity, and individual factors like motivation and life circumstances. Some individuals may need a different therapeutic modality, while others benefit from combining cognitive behavioral therapy with medication or other treatments.
Cognitive behavioral therapy CBT requires significant effort and active participation from clients. Unlike more passive forms of talk therapy, behavioral therapy involves homework assignments, practicing new behaviors between therapy sessions, and sometimes deliberately facing uncomfortable situations through exposure exercises. This demand can feel overwhelming, particularly for people experiencing severe depressive symptoms, emotional distress, or limited energy due to other medical conditions.
Access presents another practical limitation. Finding a qualified CBT therapist or other mental health professionals trained in cognitive therapy can be challenging in some areas, and waiting lists may extend for weeks or months. While online cognitive behavioral therapy options have expanded availability, not all insurance plans cover virtual treatment, and self-guided programs lack personalized support.
The cognitive model’s focus on present-day thoughts and behaviors—while one of cognitive therapy’s strengths—can also be a limitation for certain individuals. People with complex emotional trauma histories, deep-rooted emotional challenges from childhood, or personality disorders may find that cognitive behavioral therapy CBT alone doesn’t adequately address their needs. These individuals may benefit more from trauma-focused interventions, psychodynamic therapy approaches, or longer-term treatment that explores underlying behavior patterns.
We often see clients at our Dupont Circle office who initially pursue cognitive behavioral therapy because of its evidence base and efficiency, which aligns with their professional mindset. However, we’re transparent about the work involved—CBT isn’t a quick fix or a passive experience. For clients dealing with chronic pain, eating disorders, or borderline personality disorder, we frequently recommend integrating CBT techniques with other therapies to address the full complexity of their situation and enhance outcomes for their mental health.
Can CBT’s Effects Diminish Over Time?
While many people maintain long-term benefits from cognitive behavioral therapy, some individuals experience symptom return months or years after treatment ends. This is more common with certain anxiety disorders like panic disorder and generalized anxiety disorder. However, “booster sessions”—periodic check-ins with a CBT therapist—can help people refresh their coping skills and prevent full relapse when they notice early warning signs.
This pattern of gradual benefit decay contrasts with findings from psychodynamic therapy research. Multiple meta analyses have found that psychodynamic therapy benefits not only endure but actually increase over time after treatment ends—suggesting that insight-oriented approaches may set in motion psychological processes that continue working long after therapy concludes. For some people, particularly those with recurring patterns in relationships or deep-seated emotional difficulties, this difference in long-term trajectory may make psychodynamic or other exploratory therapies a better fit than cognitive behavioral therapy CBT alone.
How Does Cognitive Behavioral Therapy Compare to Other Treatments?
When directly compared to other psychotherapies and pharmacological treatments, cognitive behavioral therapy CBT performs as well as or better than many alternatives across multiple mental health conditions. Meta analyses comparing different treatments show that for depression, cognitive behavioral therapy CBT offers comparable effectiveness to antidepressant medication in the short term, with research reviews suggesting better long-term outcomes due to learned behavioral techniques and coping skills.
When people search for “types of therapy for anxiety” or explore “alternatives to CBT,” they discover that cognitive behavioral therapy CBT distinguishes itself through its structured, time-limited format and emphasis on measurable outcomes. Unlike psychodynamic therapy approaches, which explore unconscious patterns and past experiences, or interpersonal therapy, which focuses primarily on relationship dynamics, cognitive behavioral therapy CBT focuses on the specific negative thoughts and behavior patterns maintaining current mental health problems.
However, “better” depends entirely on individual needs and preferences. Some people find cognitive behavioral therapy too directive or analytical, preferring the exploratory nature of psychodynamic therapy approaches. Others need the relational focus of interpersonal therapy or the emotional regulation skills taught in dialectical behavior therapy for substance use disorders or emotional challenges in daily life.
The most effective approach for managing many mental health conditions involves combining treatments. Cognitive behavioral therapy CBT plus medication often produces superior outcomes compared to either intervention alone, particularly for moderate to severe depression and adult anxiety disorders. Meta analyses of combined treatment approaches show that CBT helps enhance outcomes when integrated with other therapies. Similarly, incorporating relaxation techniques, mindfulness practices, or family therapist involvement alongside cognitive behavioral therapy CBT can enhance outcomes for certain mental health problems, including substance use disorders.
Who Benefits Most from Cognitive Behavioral Therapy?
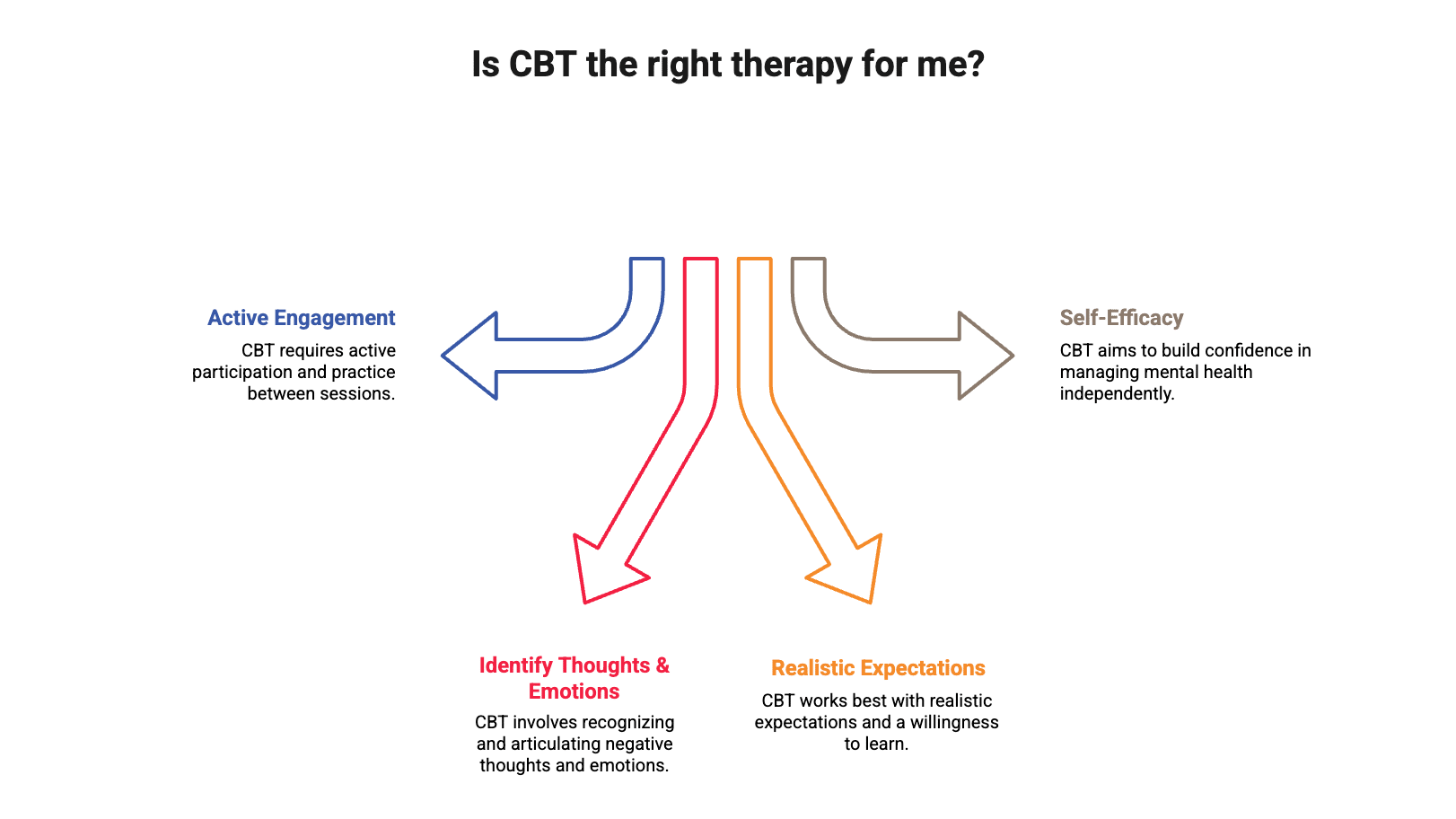
Cognitive behavioral therapy CBT tends to work best for people who are willing to actively engage in the therapeutic process, can identify and articulate negative thoughts, negative emotions, and feelings, and have the capacity to practice CBT interventions between therapy sessions. Strong evidence from meta analyses—comprehensive reviews of multiple studies—supports cognitive behavioral therapy CBT effectiveness for:
- Anxiety disorders, including generalized anxiety disorder, social anxiety disorder, social anxiety, and panic disorder
- Depression, particularly mild to moderate cases where cognitive behavioral therapy CBT helps to treat depression effectively
- Post traumatic stress disorder, especially when cognitive behavioral therapy CBT is combined with exposure therapy
- Obsessive compulsive disorder, particularly when CBT focuses on exposure with response prevention for OCD symptoms
- Eating disorders like bulimia nervosa and binge eating disorder
- Chronic pain management and chronic fatigue syndrome
- Insomnia and other sleep difficulties
- Body dysmorphic disorder and anxiety management
In our clinical experience, we regularly observe that clients who approach cognitive behavioral therapy CBT with realistic expectations and a willingness to practice skills outside sessions tend to see the strongest outcomes. We find that individuals who view therapy as an active learning process—rather than a passive “fix”—develop greater confidence in managing their mental health conditions independently. This self-efficacy often becomes one of the most valuable long-term benefits of cognitive behavioral therapy.
For those exploring different types of therapy for anxiety, cognitive behavioral therapy CBT stands out for its practical, skills-based approach. Meta analyses also demonstrate that cognitive behavioral therapy CBT works effectively with children, adolescents, and adults across diverse cultural backgrounds when appropriately adapted by trained mental health professionals.
When Might Someone Need a Different Approach?
Certain situations call for alternative or complementary therapeutic approaches. People with severe, chronic depression may need medication combined with behavioral therapy to manage depressive symptoms. Those with complex trauma or childhood abuse histories often benefit from trauma-focused interventions that go beyond standard cognitive behavioral therapy CBT. Individuals with personality disorders, particularly borderline personality disorder, typically respond better to specialized treatments like dialectical behavior therapy that emphasize emotional regulation.
People experiencing active substance use disorders, severe bipolar disorder symptoms, or psychological disorders with psychotic features generally need specialized mental health care from mental health professionals that addresses these specific challenges before or alongside CBT techniques. Bipolar disorder often requires mood-stabilizing medication before cognitive therapy approaches can be most effective.
Making an Informed Decision About CBT
Cognitive behavioral therapy CBT represents a powerful, evidence-based tool for addressing many mental health conditions, backed by decades of rigorous clinical trials. Meta analyses—large research reviews—in clinical psychology support the strengths of behavioral therapy—including practical skill-building, brief treatment timeline, and strong research support. These comprehensive research reviews make cognitive behavioral therapy CBT an excellent first-line option for people struggling with anxiety disorders, depression, and related mental health concerns.
At the same time, the limitations of cognitive behavioral therapy CBT—including the significant effort required, variable response rates, and potential need for other therapies—mean it’s not the right fit for everyone. The most important factor is finding an approach, and a mental health professional who understands how CBT helps different mental health conditions, that aligns with your specific needs and circumstances.
Get Support from Our DC Therapists
If you’re considering cognitive behavioral therapy CBT or want to discuss which therapeutic approach might work best for your situation, our doctoral-level psychologists and experienced mental health professionals at Therapy Group of DC can help. We offer evidence-based treatment tailored to your unique needs, including cognitive behavioral therapy CBT, cognitive behavioural therapy, cognitive therapy, and other therapeutic modalities. Contact us to schedule a consultation and take the first step toward better mental health.
This blog provides general information and discussions about mental health and related subjects. The content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.